- Introduction
- Chapter I - Online System Terminology
- Chapter II - Online Menu Functions Overview
- Chapter III - Navigating the Online System
-
Chapter IV - Inquiries Submenu (01)
- Accessing the Inquiries Submenu
- Beneficiary/CWF (10)
- DRG (Pricer/Grouper) (11)
- Claim Summary (12)
- Revenue Codes (13)
- HCPCS Codes (14)
- DX/Proc Codes ICD-9 (15)
- Adjustment Reason Codes (16)
- Reason Codes (17)
- ZIP Code File (19)
- OSC Repository Inquiry (1A)
- Claim Count Summary (56)
- Home Health Payment Totals (67)
- ANSI Reason Codes (68)
- Invoice Number/DCN Translator (88)
- DX Proc Codes ICD-10 (1B)
- Community Mental Health Centers Services Payment Totals (1C)
- Check History (FI)
- Provider Practice Address Query (1D)
- New HCPCS Screen (1E)
- Opioid Use Disorder (OUD) Demo 99 (1F)
- Chapter V - Claims and Attachments Submenu (02)
- Chapter VI - Claims Correction Submenu (03)
- Chapter VII - Online Reports View Submenu (04)
-
Resources
- Part A Electronic Medicare Secondary and Tertiary Payer Specifications for ANSI Inbound Claim
- Electronic Medicare Secondary Payer Specifications for Inbound Claims
- FISS UB-04 Data Entry Payer Codes
- Common Claim Status/Locations
- FISS Reason Code Overview
- FISS Reason Code/Claim Driver Overview
- Program Function/Escape Key Crosswalk
- How to Adjust a Claim
- FISS Claim Change/Condition Reason Codes
- How to Cancel a Claim
- How to Correct a Return to Provider Claim
- Online System Menu Quick-Reference
Chapter V: Claims/Attachments Submenu (02)
Claim Data Entry
Purpose
The Claims Entry options allows the provider to enter claims and roster bills electronically into the FISS DDE Provider Online System.
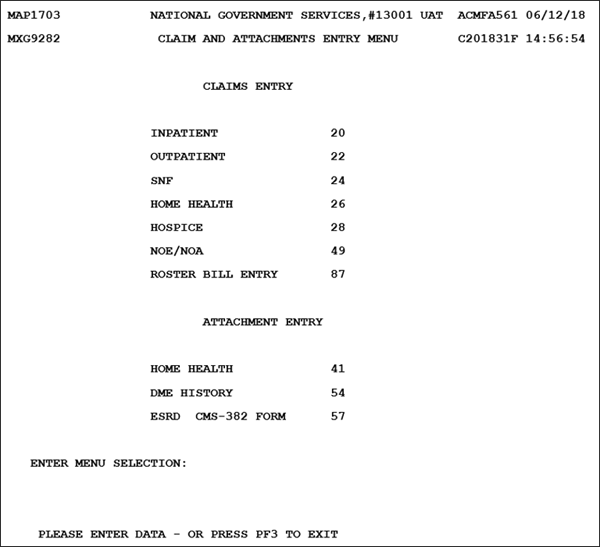
To initiate claim data entry (other than roster bill entry), from the Claims Entry options, key the option number that represents the type of claim that you wish to enter at the Enter Menu Selection: prompt, then press <Enter>.
Upon selecting the Claims Entry option, Claim Page 01 is available:
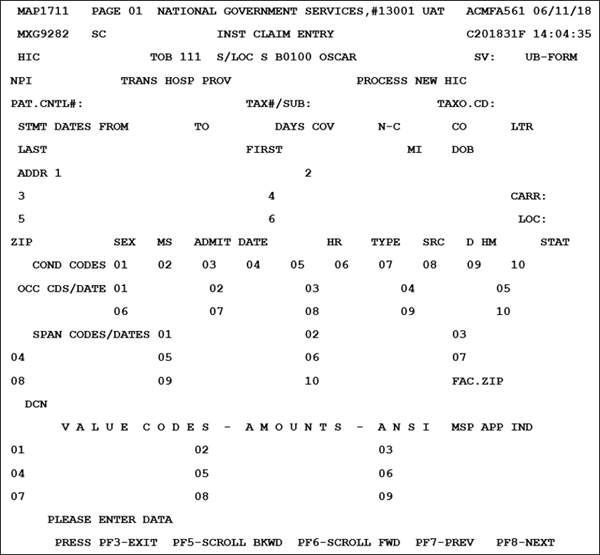
Entering Claim Data
The data entry screens are set up to look similar to a UB-04 claim form. There are six pages to a claim.
- Claim page 01 corresponds to locators 1–41 of the UB-04.
- Claim page 02 corresponds to locators 42–49 of the UB-04.
- Claim page 03 corresponds to locators 50–57 and 66–79 of the UB-04.
- Claim page 04 corresponds to locator 80 of the UB-04.
- Claim page 05 corresponds to locators 58–65 of the UB-04.
- Claim page 06 corresponds to locators 67–69 of the UB-04.
Note: NUBC maintains the UB-04 data element specifications. NUBC may be contacted for subscription on the NUBC website.
To begin claim data entry, key in the following fields and use the <Tab> key to advance to the next field. Depending on the type of bill, the cursor may skip fields that are not required.
- Providers that have multiple logons for their acute and exempt units must logoff the system and logon under their appropriate NPI number.
| Field | Description |
|---|---|
| MID | Medicare ID Number (12-position alphanumeric field) |
| TOB | Type of Bill – Identifies the type of facility, bill classification, and frequency of the claim (three-position alphanumeric field) Note: The online system defaults to TOB 111 for inpatient, 131 for outpatient, and 211 for SNF. If entering data for a different bill type, overkey the TOB field with the correct type of bill. |
| S/LOC | Status/Location – automatically filled in upon selecting the appropriate claim entry bill type |
| OSCAR | Medicare OSCAR (provider) number – automatically filled in (ten-position alphanumeric field) |
| SV | Suppress View – only accessible in Claim Correction mode |
| UB-FORM | Identifies the type of claims to be processed in this batch (one-position field) Valid value A = UB-04 |
| NPI | NPI number (ten-position alphanumeric field) |
| TRAN HOSP PROV | Transferring Hospice Provider – Displays the identification number of the institution which rendered services to the beneficiary/patient (13-position alphanumeric field) |
| PROCESS NEW MID | Process New MID – only accessible in Claim Correction mode. |
| PAT.CNTL# | Patient Control Number – patient’s number assigned by the provider to facilitate retrieval of individual patient records and posting of the payment (20-position alphanumeric field) |
| TAX#/SUB | Tax ID Number – number assigned to the provider by the federal government for tax reporting purposes. It is also known as a TIN or an EIN (ten-position alphanumeric field) Tax Subsidiaries – affiliated subsidiaries associated to the provider of services (four-position alphanumeric field) |
| TAXO. CD | Taxonomy Code–collection of unique alphanumeric codes. The code set is structured into three distinct “levels” including provider type, classification, and area of specialization (ten-position alphanumeric field) |
| STMT DATES FROM TO |
Statement Dates From – beginning DOS (six-position alphanumeric field in MMDDYY format) Statement Dates To – ending DOS (six-position alphanumeric field in MMDDYY format) |
| DAYS COV | Number of Days Covered by Medicare (three-position field) Valid values 000–999 |
| N-C | Number of Noncovered Days (four-position field) Valid values 0000–9990 |
| CO | Number of Coinsurance Days – inpatient Medicare days occurring after the 60th day and before the 91st day in a single spell of illness Valid values 00–60 |
| LTR | Lifetime Reserve Days used – Under the Medicare Program, each beneficiary has a lifetime reserve of 60 additional days of inpatient hospital services after using 90 days of inpatient hospital services during a spell of illness (three-position field) Valid values 000–060 |
| LAST | Patient’s Last Name at the time services were rendered (20-position alphanumeric field—spaces and special characters are prohibited for this field) |
| FIRST | Patient’s First Name (ten-position alphanumeric field) |
| MI | Patient’s Middle Initial (one-position alphanumeric field—spaces are allowed in this field) |
| DOB | Patient’s Date of Birth (eight-position field in MMDDYYYY format) |
| ADDR | Patient’s street Address including house number, P.O. box number, and/or apartment number, the patient’s city address, and the patient’s state address abbreviation (30-position alphanumeric field, with six occurrences) Note: The state abbreviation must be a valid state abbreviation accepted by the U.S. Postal Service. |
| CARR | Value Codes Carrier Number – identification number of the Medicare carrier (five-position alphanumeric field) Note: The carrier information is associated with the nine-position ZIP Code reported in the FAC.ZIP field. See Chapter IV: Inquiries Submenu (01) ZIP Code File (19) to research the carrier code for your location. |
| LOC | Value Codes Locality Code – specific location of a provider of services in a given state falling under the realm of a particular carrier’s jurisdiction (two-position alphanumeric field) Note: The locality information is associated with the nine-position ZIP Code reported in the FAC.ZIP field. See Chapter IV: Inquiries Submenu (01) ZIP Code File (19) to research the carrier code for your location. |
| ZIP | Patient’s ZIP Code (nine-digit numeric field) |
| SEX | Patient’s Sex as recorded at the time services were rendered (one-position alphanumeric field) Valid values M = Male F = Female U = Unknown |
| MS | Patient’s Marital Status at the time services were rendered (one-position alphanumeric field) Valid values S = Single M = Married X = Legally separated D = Divorced W = Widowed U = Unknown |
| ADMIT DATE | Admission Date – date of the patient’s admission to this provider or the date home health services began (six-position alphanumeric field in MMDDYY format) |
| HR | Admission Hour and Minutes – hour and minutes at which the patient was admitted for inpatient or outpatient care. Enter the hour and minutes (military time) or enter ‘99’ if unknown (four-position field in HHMM format) |
| TYPE | Admission type – code indicating the priority of admission (one-position alphanumeric field) Valid Values: 1 – Emergency 2 – Urgent 3 – Elective 4 – Newborn 5 – Trauma Center |
| SRC | Source of Admission – the way a patient was referred to the hospital for admission (one-position alphanumeric field) Valid Values: 1 – Physician referral 2 – Clinical referral 3 – HMO (Health Maintenance Organization) referral 4 – Transfer from a hospital 5 – Transfer from a SNF (Skilled Nursing Facility) 6 – Transfer from another health care facility 7 – Emergency room 8 – Court/law enforcement 9 – Information not available A – Transfer from a Critical Access Hospital (CAH) B – Transfer from another Home Health Agency C – Readmission to the same Home Health Agency D – Transfer from hospital inpatient in the same facility resulting in a separate claim to the payer – The patient was admitted to this facility as a transfer from hospital inpatient within this facility resulting in a separate claim to the payer. E – Transfer from Ambulatory Surgical Center F – Transfer from Hospice and is Under a Hospice Plan of Care or Enrolled in Hospice Program |
| D HM | Discharge Hour and Minutes – hour and minutes that the patient was discharged from inpatient care. Enter the hour and minutes (military time) or use ‘99’ if unknown (four-position field in HHMM format) |
| STAT | Patient Status code – indicates the patient’s status at the ending DOS in the period (two-position alphanumeric field) |
| COND CODES | Condition Codes – used to identify conditions relating to the claim that may affect payer processing. Up to 30 codes may be used. Use the <F6/PF6> key to enter additional condition codes (two-position alphanumeric field) |
| OCC CDS/DATES | Occurrence Codes and Dates – identify significant events relating to payment of the claim. Up to 30 pairs of codes and dates may be used. Use the <F6/PF6> key to enter additional occurrence codes and dates (occurrence code is two-position alphanumeric; date is six-position field in MMDDYY format) |
| OCCURRENCE SPAN AND DATE | Occurrence Span Codes and Dates (From/Through) – identify events that relate to the payment of the claim that span several days. The dates identify the commencement and ending of an event that relates to the payment of the claim. Up to ten sets of codes and dates may be used (occurrence span code is two-position alphanumeric field; dates are six-position fields in MMDDYY format) |
| FAC.ZIP | Facility ZIP Code – provider or subpart ZIP Code (nine-position numeric field) |
| DCN | Document control number – identification number of the claim (23-position alphanumeric field) |
| VALUE CODES | Value Codes – identify data of a monetary nature that is necessary for processing the claim as qualified by payor organizations. Up to 36 value codes may be reported. Use the <F6/PF6> key to enter additional value codes (two-position alphanumeric This field is also used to reflect the number of therapy visits based on certain value codes. |
| AMOUNTS | Value Codes Amounts – dollar amount associated with reported value code. Up to 36 value code amounts may be reported. Use the <F6/PF6> key to enter additional value code amounts (11-position numeric in ########.## format). This field is also used to reflect the number of therapy visits based on certain value codes. |
| ANSI | ANSI Codes – American National Standards Institute (ANSI) codes associated with the value code amount. The ANSI codes and amounts are forwarded to the financial system for remittance processing. Up to 36 ANSI codes may be reported. Use the <F6/PF6> key to enter additional ANSI codes (ANSI group codes are two-position alphanumeric; ANSI adjustment reason codes are three-positions alphanumeric) |
| MSP APP IND | MSP Apportion Indicator – Identifies to the Medicare Secondary Payer (MSP) PAY module whether the system apportions the primary payer’s amount and the obligated to accept as payment in full amount (OTAF) amounts (if present) (one-position alphanumeric field) Valid values ‘ ’ = Apportion N = Do not apportion. Note Allows entry into the Payer 1, Payer 2, OTAF and Denial Indicator fields on MAP171A. Note: The user will be responsible for entering the other payer amount, per line item. |
After keying all the Claim Page 01 information, press the <F8/PF8> key to access Claim Page 02.
Note: If the <F3>/<PF3> key is pressed while entering data from the claim (before the claim has been submitted by pressing <F9>/<PF9>), all the information you just keyed will be lost.
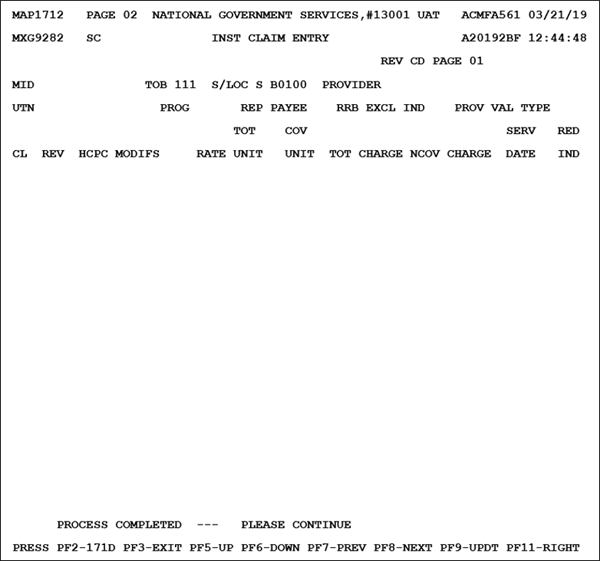
Use Claim Page 02 to report line item details. To insert a revenue code line, key in the claim line details and press the <Enter> key. The system will store the claim line and prepare to accept a new revenue code line.
Up to 450 revenue code lines can be reported per claim. 14 revenue code lines are available per page. Use the <F6/PF6> and <F5</<PF5> keys to access additional revenue code screens.
List revenue codes in ascending numeric sequence.
Note: Type in the dollar amounts without a decimal point (e.g., for $45.50 type ‘4550’).
To limit the number of line item entries on each bill, report each revenue code only once, except when distinct HCPCS code reporting requires repeating a revenue code (i.e., laboratory services—revenue code 300—repeated with different HCPCS codes), or an accommodation revenue code requires repeating with a different rate.
Revenue code 0001 (Total Charges) should always be the final revenue code line. The sums for all the reported totals for TOTAL CHARGES and NONCOVERED CHARGES on the claim should be reported on the 0001 line.
Note: The FISS DDE online system does not recalculate the total or noncovered charges associated with revenue code 0001. Providers need to ensure the accuracy of these totals before submitting the claim.
| Field | Description |
|---|---|
| REV CD PAGE | Shows Revenue Code Page sequence |
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Status/Location code (system generated from Claim Page 01) |
| PROVIDER | Provider number (system generated from Claim Page 01) |
| UTN | Unique Tracking Number that is submitted on the claim in the Medicare Treatment Authorization field (14-position alphanumeric field) |
| PROG | Prior Authorization Program ID matching to the item/services submitted on the claim (four-position alphanumeric field in ANNN or HNNN format) |
| REP PAYEE | Identifies a Medicare Beneficiary with a Rep Payee (one-position alphanumeric field) Valid Values: R – Bypass Rep Payee Blank – Rep Payee processing does not apply |
| RRB EXCL IND | Railroad Board (RRB) Beneficiary Indicator (one-position alphabetic field) Valid Values: Y – Exclude RRB Beneficiary from Prior Authorization services Blank – Beneficiary services are subject to Prior Authorization |
| PROV VAL TYPE | Designated Provider Validation Type (two-position alphabetic field) Valid Values: AP – Attending Physician CP – Ordering/Referring Physician FA – Facility OP – Operating Physician RP – Rendering Physician Blank – Designated Provider processing does not apply |
| CL | Claim line (system generated) |
| REV | Revenue code (four-position numeric) |
| HCPC | HCPCS code to identify procedure/service rendered (five-position alphanumeric) |
| MODIFS | Modifier code (two-position alphanumeric) Note: additional modifiers can be entered on Claim Page 02, Right View using the <F11/PF11> key. |
| RATE | Per unit Rate for line item (nine-position numeric field in ######.## format) |
| TOT UNIT | Total Units of Service rendered (four-position numeric) |
| COV UNIT | Total Covered Units rendered (four-position numeric) |
| TOT CHARGE | Total Charges (11-position numeric in ########.## format) |
| NCOV CHARGE | Noncovered Charges (11-position numeric in ########.## format) |
| SERV DATE | Date of Service – reported by hospitals and CMHCs for every line where a HCPCS code is required. Required on all laboratory claims (six-position numeric field in MMDDYY format) Note: for IRF PPS claims, the date of service is not required on the revenue code 0024 line. However, if present on the revenue code 0024 line, it indicates the date the provider transmitted the patient assessment and must be equal to or greater than the discharge (STATEMENT COVERS TO) date. |
| RED IND | Identifies if the payment for the line was paid using the therapy reduced rate (one-position alpha field) Valid Values: F – 100% Reimbursement for multiple surgical or endoscopic procedures. M – Partial Reimbursement for multiple surgical or endoscopic procedures. P – Partial, all of the units except one were reduced R – All units were reduced Blank – Default |
Deleting a Revenue Code Line
- Tab down to the revenue code line that you wish to delete and place a ‘DDD’ in the first, second and third position of the revenue code.
- Press the <Home> key.
- Press the <Enter> key.
This will delete the entire revenue code line.
Please note: NUBC maintains the revenue code tables. NUBC may be contacted for subscription to the UB-04 on the NUBC website.
After keying line item detail, press the <F11/PF11> key to access Claim Page 02, First Right View – National Drug Code:
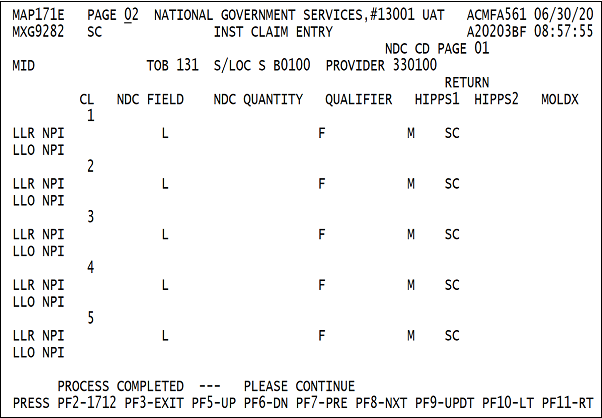
This screen will only be used when the HCPCS code C9399 is keyed. The system will prompt you when to key in the appropriate NDC. In addition, the MOLDX field identifies the unique test ID.
| Field | Description |
|---|---|
| NCD CD PAGE | Shows National Drug Code Page sequence |
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Status/Location code (system generated from Claim Page 01) |
| PROVIDER | Provider number (system generated from Claim Page 01) |
| CL | Claim line number |
| NDC FIELD | Identifies the National Drug Code (11-position numeric field) |
| NDC QUANTITY | Identifies the NDC Quantity (12-position numeric field in ########.### format) |
| QUALIFIER | Identifies the NDC quantity qualifier (two-position alphanumeric field) |
| RETURN HIPPS1 | Identifies the first HIPPS code returned from the QIES Response file (five-position alphanumeric field) |
| RETURN HIPPS2 | Identifies the second HIPPS code returned from the QIES Response file (five-position alphanumeric field) |
| MOLDX | Identifies the Molecular Diagnostic Services test ID (five-position alphanumeric field) |
| LLR NPI | Identifies the Line Level Rendering Physician's NPI (National Provider Identifier) number (ten-position alphanumeric field) |
| LLO NPI | Identifies the Line Level Ordering Provider’s NPI (National Provider Identifier) number (ten-position alphanumeric field) |
| L | Identifies the Last Name of the physician (17-position alpha field) |
| F | Identifies the First Name of the physician (eight-position alpha field) |
| M | Identifies the Middle Initial of the physician (a one-position alpha field) |
| SC | Identifies the Physician Specialty Code (two-position alphanumeric field) |
After keying NDC information, press the <F11/PF11> key to access Claim Page 02, Second Right View:
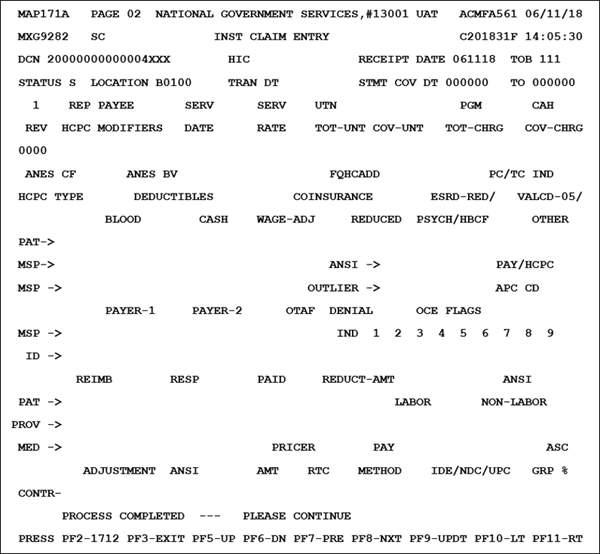
| Field | Description |
|---|---|
| DCN | Document Control Number (23-position alphanumeric field) |
| MID | Medicare ID Number (system generated from Claim Page 01) |
| RECEIPT DATE | Date claim received |
| TOB | Type of bill (system generated from Claim Page 01) |
| STATUS | Current Status of claim |
| LOCATION | Current Location of claim |
| TRAN DT | Last Transaction Date – last date status/location changed or claim was updated |
| STMT COV DT | Statement Covers Date (FROM) – beginning DOS |
| TO | Statement Covers Date (TO) – end DOS |
| 1 | This field identifies the line number of the revenue code. The line number is located above the revenue code on this screen. To move to another revenue code, enter the new line number and press the <Enter> key. |
| REP PAYEE | Identifies a Medicare Beneficiary with a Rep Payee (one-position alphanumeric field) Valid Values: R ‒ Bypass Rep Payee Blank ‒ Rep Payee processing does not apply |
| UTN | Identifies the Unique Tracking Number (UTN) that is submitted on the claim in the Medicare Treatment Authorization field (14-position alphanumeric field) |
| PGM | Identifies the Prior Authorization Program ID matching to the item/services submitted on the claim (four-position alphanumeric field in ANNN or HNNN format) |
| CAH | CAH Incentive Indicator – identifies whether a claim line is eligible for a specific type of bonus. This is a one-position alphanumeric field. Valid Values: 1 – HPSA 2 – PSA 3 – HPSA and PSA 4 – HSIP 5 – HPSA and HSIP 6 – PCIP 7 – HPSA and PCIP Blank ‒ Not applicable Note: The system determines the bonus eligibility status of the line based on the Offsite Zip Code field on MAP1034. |
| REV | Revenue code as reported on Claim Page 02 |
| HCPC | HCPCS code as reported on Claim Page 02 |
| MODIFIERS | HCPCS modifier codes for claims processing. The two modifiers entered on Claim page 02 are displayed and the user can enter any remaining modifiers (ten-position alphanumeric field to contain five two-position modifiers) |
| SERV DATE | Line item date of service as reported on Claim Page 02 |
| SERV RATE | Per unit cost as reported on Claim Page 02 |
| TOT-UNT | Total Units billed as reported on Claim Page 02 |
| COV-UNT | Total Covered Units billed as reported on Claim Page 02 |
| TOT-CHRG | Total Charges as reported on Claim Page 02 |
| COV-CHRG | Total Covered Charges as reported on Claim Page 02 |
| ANES CF | Identifies the Anesthesia Conversion Factor (five-position numeric field in ##.## format) |
| ANES BV | Identifies the Anesthesia Base Unit Value (three-position numeric field) Valid Values: 001‒199 |
| FQHCADD | Identifies the FQHC new patient/IPPE/AWV add on payment amount |
| PC/TC IND | Identifies the Professional Component/Technical Component (PC/TC) indicator that is added to the CORF extract of the Medicare Physician Fee Schedule Supplementary File. This is used to identify professional services eligible for the HPSA bonus payments. This field is only applicable when pricing CAHs) that have elected the optional method (Method 2) of payment. |
| HCPC TYPE | Identifies whether the HCPCS originated from the MPFS database files and it paid off the fee rate (one-position alphanumeric field) Valid Values: M ‒ Originated from MPFS database files Blank ‒ Did not originate from the MPFS database files |
| PAT BLOOD DEDUCTIBLES | Identifies the amount of the patient’s Medicare blood deductible applied to the line item. The blood deductible is applied at the line level on revenue codes 380, 381, and 382 (11-position numeric field in 99999999.99 format) |
| PAT CASH DEDUCTIBLES | Identifies the amount of the patient’s Medicare cash deductible applied to the line item (11-position numeric field in 99999999.99 format) |
| WAGE ADJ COINSURANCE | Identifies the amount of coinsurance applicable to the line, based on the particular service rendered. The service is defined by the revenue and HCPCS code submitted. For services subject to OPPS in hospitals (TOBs 12X, 13X and 14X) and in community mental health centers (TOB 76X), the applicable coinsurance is wage adjusted. This field will have either a zero (for services which no coinsurance is applicable), or a regular coinsurance amount (calculated on either charges or a fee schedule) unless the service is subject to OPPS. If the service is subject to OPPS, the national coinsurance amount will be wage adjusted based on the MSA where the provider is located or assigned as the result of a reclassification. CMS supplies the national coinsurance amount to the MACS, as well as the MSA by provider (11 eleven-position numeric field in 99999999.99 format) |
| REDUCED COINSURANCE | Identifies the amount of the reduced coinsurance applicable to the line for a particular service (HCPCS) rendered on which the provider has elected to reduce the coinsurance amount for all services subject to OPPS (TOB 12X, 13X, 14X, 76X). (11-position numeric field in 99999999.99 format) Note: Providers are only permitted to reduce the coinsurance amount due from the beneficiary for services paid under OPPS, and the reduced amount cannot be lower than 20% of the payment rate for the line. If the provider does not elect to reduce the coinsurance amount, this field will contain zeros. |
| ESRD ‒RED/PSYCH/HBCF | Identifies the ESRD Reduction Amount/Psychiatric Reduction Amount/Hemophilia Blood Clotting Factor Amount (12-position numeric field in 999999999.99 format) ESRD Reduction Amount – refers to the ESRD Network Reduction amount. Psychiatric Reduction Amount – Applies to line items that have a P Pricing Indicator. The amount represents the psychiatric coinsurance amount (37.5% of covered charges). Hemophilia Blood Clotting Factor Amount – An additional payment to the DRG payment for hemophilia. The payment is based on the applicable HCPC and add-on applies to inpatient claims. |
| VALCD-05/OTHER | Identifies whether Value Code 05 is present on the claim. It contains the portion of the value code 05 amount that is applicable to this line item. The value code 05 amount is first applied to revenue codes 96X, 97X, 98X and then applied to revenue code lines in numeric order that are subject to deductible and/or coinsurance (ten-position numeric field in 9999999.99 format) |
| MSP BLOOD DEDUCTIBLES | Identifies the Blood Deduction amount calculated within the MSPPAY module and apportioned upon return from the MSPPAY module (ten-position numeric field in 9999999.99 format) |
| MSP CASH DEDUCTIBLES | Identifies the Cash Deduction amount calculated within the MSPPAY module and apportioned upon return from the MSPPAY module (eight-position numeric field in 99999.99 format) |
| MSP COINSURANCE | Identifies the Coinsurance amount calculated within the MSPPAY module and apportioned upon return from the MSPPAY module (eight-position numeric field in 99999.99 format) |
| ANSI ESRD-RED/PSYCH/HBCF | Identifies the two-position ANSI group code and three-position ANSI reason (adjustment) code. The ANSI data for the value codes are sent to the financial system for reporting on the remittance advice for the ESRD Reduction/Psychiatric Coinsurance/Hemophilia Blood Clotting Factor. |
| ANSI VALUECD-05/OTHER | Identifies the two-position ANSI group code and three-position ANSI reason (adjustment) code. The ANSI data for the value codes are sent to the financial system for reporting on the remittance advice for the Value Code 05/Other amount. |
| OUTLIER | Identifies the apportioned line level Outlier amount returned from MSPPAYOL (ten-position numeric field in 9999999.99 format) |
| PAY/HCPC APC CD | Identifies the Payment APC Code or HCPC APC Code. This field displays the number that identifies the APC group. Payment for services under OPPS is calculated based on grouping outpatient services into APC groups. The payment rate and coinsurance amount calculated for an APC apply to all of the services within the APC. Both APC codes appear on the claims file, but only one displays on the screen. If their values are different, this indicates a partial hospitalization item. In this case the payment APC code is displayed. When the item is not a partial hospitalization, the HCPC APC code is displayed. This data is read from the claims file (five-position alphanumeric field) |
| MSP PAYER-1 | Identifies the amount entered by the user (if available) or apportioned by MSPPAY as Payment from the Primary Payer. The MSPPAY Module based on the amount in the value code for the primary payer apportions this amount (ten-position numeric field in 9999999.99 format) |
| MSP PAYER-2 | Identifies the amount entered by the user (if available) or apportioned by MSPPAY as Payment from the Secondary Payer. The MSPPAY Module based on the amount in the value code for the primary payer apportions this amount (ten-position numeric field in 9999999.99 format) |
| OTAF | Identifies the line item apportioned amount calculated by the MSPPAY module of the Obligated to Accept as Payment in Full, when value code 44 is present (ten-position numeric field in 9999999.99 format) |
| ID PAYER 1 | One-position alphanumeric code identifying the specific payer. If Medicare is primary, this field is blank. |
| ID PAYER 2 | One-position alphanumeric code identifying the specific payer. If Medicare is secondary, this field is blank. |
| DENIAL IND | Denial Indicator - identifies to the MSPPAY module that an insurer primary to Medicare has denied this line item (one-position alphanumeric field) Valid Values: D – Denied Blank – Not denied |
| OCE FLAGS 1 2 3 4 5 6 7 8 9 |
Identifies nine OCE flags (two-positon alphanumeric each) |
| REDUCT-AMT | Reduction Amount – identifies the 10% reduction amount by a processed 121 re-billed demonstration claim that paid 90% of allowable services identified by including CARC 45 to report the adjustment due to difference in billed charged and allowed amount, and CARC 132 to report adjustments due to a 10% reduction in conjunction with Group Code of CO (ten-position alphanumeric field in 99999999.99 format) Valid Values: 45 – Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement. 132 – Prearranged demonstration project adjustment. |
| ANSI | Identifies the ANSI group code and the CARC code for the reduction amount above (group code is a two-position alphanumeric field; CARC code is a three-position alphanumeric field) |
| PAT REIMB | Patient Reimbursement – identifies the system generated calculated line amount to be paid to the patient on the basis of the amount entered by the provider on claim page four, in the Due From PAT field (11-position numeric field in 99999999.99 format) |
| PAT RESP | Patient Responsibility – identifies the amount for which the individual receiving services is responsible (eleven-position numeric field in 99999999.99 format). The amount is calculated as follows: If Payer 1 indicator is C or Z, then the amount equals: cash deductible + coinsurance + blood deductible. If Payer 1 indicator is not C or Z, then the amount equals: MSP blood + MSP cash deductible + MSP coinsurance. |
| PAT PAID | Patient Paid – identifies the line item patient paid amount calculated by the system. This amount is the lower of (patient reimbursement + patient responsibility) or the remaining patient paid (after the preceding lines have reduced the amount entered on claim page 4) (ten-position numeric field in 9999999.99 format) |
| PROV REIMB | Provider Reimbursement – identifies the system calculated line item amount to be paid to the provider (11-position numeric field in 99999999.99 format) |
| LABOR | Identifies the Labor Amount of the payment as calculated by the pricer (nine-position numeric field in 999999.99 format) |
| NON-LABOR | Identifies the Nonlabor Amount of the payment as calculated by the pricer (nine-position numeric field in 999999.99 format) |
| MED REIMB | Identifies the total Medicare Reimbursement for the line item, which is the sum of the patient reimbursement and the provider reimbursement (11-position numeric field in 99999999.99 format) |
| CONTR ADJUSTMENT | Identifies the total Contractual Adjustment. The calculation is: submitted charge – deductible – wage adjusted coinsurance – blood deductible – value code 71 – psychiatric reduction – value code 05/other – reimbursement amount (11-position numeric field in 99999999.99 format) Note: For MSP Claims, the MSP deductible, MSP blood deductible, and MSP coinsurance are used in the above calculation in place of the deductible, blood deductible, and coinsurance amounts. |
| PRICER AMT | Identifies the Total Reimbursement Received from a Pricer (11-position numeric field in 99999999.99 format) |
| PRICER RTC | Identifies the Return Code from OPPS (two-position alphanumeric field) |
| PAY METHOD | Identifies the payment method returned from OCE. This is two-position alphanumeric field. Valid Values: 1 – Paid standard OPPS amount (status indicators K, S, T, V, X or P) 2 – Services not paid under OPPS (status indicator A) 3 – Not paid (status indicators W, Y or E) or not paid under OPPS (status indicators B, C, Z) 4 – Acquisition cost paid (status indicator F or L) 5 – Additional payment for drug or biological (status indicator G) 6 – Additional payment for device (status indicator H) 7 – Additional payment for new drug or new biological (status indicator J) 8 – Paid partial hospitalization per diem (status indicator P) 9 – therapy, or G0177 (partial hospitalization program services) |
| IDE/NDC/UPC | Identifies the IDE (Investigational Device Exemption), NDC, or UPC authorization number assigned by the FDA (15-position alphanumeric field) |
| ASC GROUP | Identifies the ASC Group code for the indicated revenue code (three-position alphanumeric field) |
| ASC % | Identifies the Percentage Used by the ASC Pricer in its calculation for the indicated revenue code (one-position numeric field) |
Press the <F11/PF11> key to access Claim Page 02, Third Right View:
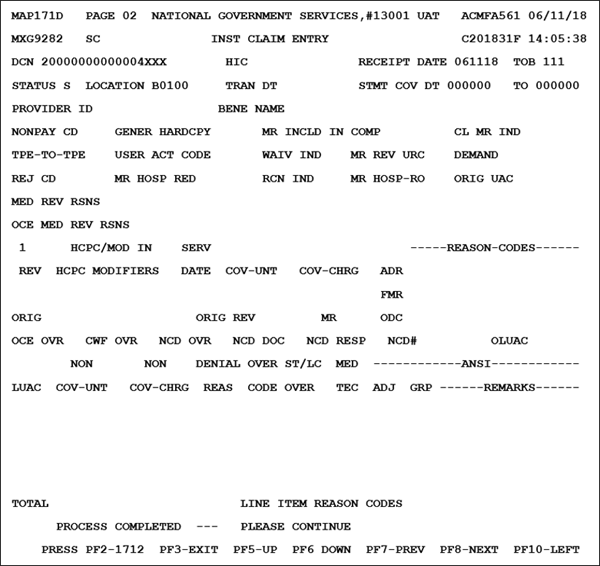
Note: The Claim Page 02 Third Right View screen was added to the FISS DDE Provider Online System for providers to view in inquiry mode only.
| Field | Description |
|---|---|
| DCN | Document Control Number (23-position alphanumeric field) |
| MID | Medicare ID Number (system generated from Claim Page 01) |
| RECEIPT DATE | Date claim received |
| TOB | Type of bill (system generated from Claim Page 01) |
| STATUS | Current Status of claim |
| LOCATION | Current Location of claim |
| TRAN DT | Last Transaction Date – last date status/location changed or claim was updated |
| STMT COV DT | Statement Covers Date (FROM) – beginning DOS |
| TO | Statement Covers Date (TO) – end DOS |
| PROVIDER ID | Provider NPI (13-position alphanumeric field) |
| BENE NAME | Name of the Beneficiary (30-position alphanumeric field) |
| NONPAY CD | Identifies the reason for Medicare’s decision not to make payment (two-position alphanumeric field) |
| GENER HARDCPY | Instructs the system to generate a specific type of hard copy document (one-position alphanumeric field) |
| MR INCLD IN COMP | Identifies (for ESRD bills) if the claim has been denied because the service should have been included in the Composite Medical Review Rate (one-position alphanumeric field) Valid Value: Y ‒ The claim has been denied |
| CL MR IND | Identifies if all services on the claim received complex manual medical review. The value entered in this field auto-populates the MR IND field for all revenue code lines on the claim (one-position alphanumeric field) Valid Values: Blank ‒ The services did not receive manual medical review (default value) Y ‒ Medical records received. This service received complex manual medical review N ‒ Medical records were not received. This service received routine manual medical review |
| TPE-TO-TPE | Identifies the tape-to-tape flag, if applicable (one-position alphanumeric field) The valid values are the flag indicators across the top of the chart. Each indicator instructs the system to either perform or skip each of the four functions listed on the left of the chart. The first indicator column represents a blank. If this field is blank, all functions are performed (as indicated on the chart). |
| USER ACT CODE | User Action Code is to be used for medical review and reconsideration only. First position: User Action Code Second position: Reconsideration Code. The reconsideration user action code will always be R. When a recon is performed on the claim, the user should enter an R in the second position of the claim user action code, or in the line user action code field. This tells the system that reconsideration has been performed (two-position alphanumeric field) |
| WAIV IND | Identifies whether the provider has their presumptive waiver status (one-position alphanumeric field) Valid Values: Y ‒ The provider does have their waiver status. N ‒ The provider does not have their waiver status. |
| MR REV URC | Identifies whether a Skilled Nursing Facility Utilization Review Committee (SNF URC) Claim has been reversed. This indicator can be used for a partial or a full reversal (one-position alphanumeric field) Valid Values: P ‒ Partial reversal F ‒ Full reversal, the system reverses all charges and days. |
| DEMAND | Identifies if a SNF demand claim has been reversed (one-position alphanumeric field) Valid Values: P ‒ Partial reversal, it is the operators responsibility to reverse the charges and days to reflect the reversal. F ‒ Full reversal, the system reverses all charges and days. |
| REJ CD | Identifies the reason code for which the claim is being denied (five-position alphanumeric field) |
| MR HOSP RED | Identifies (for hospice bills) the line item(s) that have been reduced to a lesser charge by medical review (one-position alphanumeric field) Valid Values: Y – Reduced Blank ‒ Not reduced |
| RCN IND | Reconsideration Indicator - used only for home health claims (one-position alphanumeric field) Valid Values: A ‒ Finalized count affirmed B ‒ Finalized no adjustment count (pay per waiver) R ‒ Finalized count reversal (adjustment) U ‒ Reconsideration |
| MR HOSP-RO | Identifies (for RO Hospice bills) if the claim has been referred to the Regional Office for questionable revocation (one-position alphanumeric field) Valid Values: Y ‒ Referred Blank ‒ Not referred |
| ORIG UAC | Original User Action Code ‒ populated/updated when the claim level user action code is populated/updated (two-position alphanumeric field) |
| MED REV RSNS | Identifies a specific error condition relative to medical review. There are up to ten medical review reasons that can be captured per claim. This field displays Medical Review Reasons specific to claim level. The system determines this by a C in the claim/line indicator on the reason code file. The medical review reasons must contain a 5 in the first position (five-position alphanumeric field) |
| OCE MED REV RSNS | Identifies the edit returned from the OPPS version of OCE (three-position alphanumeric field) Valid Values: 11 ‒ Noncovered service submitted for review (condition code 20). 12 ‒ Questionable covered service. 30 ‒ Insufficient services on day of partialization. 31 ‒ Partial hospitalization on same day as electro convulsive therapy or type T procedure. 32 ‒ Partial hospitalization claim spans three or less days with insufficient services, or electro convulsive therapy or significant procedure on at least one of the days. 33 ‒ Partial hospitalization claim spans more than 3 days with insufficient number of days having mental health services. |
| 1 | Identifies the line number of the revenue code (three-positon numeric field). The line number is located above the revenue code on this page. To move to another revenue code, enter the new line number and press the <Enter> key. |
| HCPC/MOD IN | Identifies whether the HCPC Code, Modifier, or the REV Code were changed (one-position alphanumeric field). Valid Values: U ‒ Upcoding D ‒ Downcoding Blank ‒ Blank |
| ADR REASON-CODES | Identifies the ADR reason codes that are present on the screen (five-position alphanumeric field) |
| REV | Identifies the Revenue Code for a specific accommodation or service that was billed on the claim (this information was entered on Claim Page 02) |
| HCPC | Identifies the HCPC code that further defines the revenue code being submitted (this information on this field was entered on Claim Page 02) |
| MODIFIERS | Identifies the HCPCS modifier codes for claims processing (ten-position alphanumeric field; can contain five two-position alphanumeric modifiers) |
| SERV DATE | Line item date of service ‒ required for many outpatient bills. This information was entered on Claim Page 02 (six-position alphanumeric field in MMDDYY format) |
| COV-UNT | Number of covered units associated with the revenue code line item being denied (seven-position numeric field in 9999999 format) |
| COV-CHRG | Number of covered charges associated with the revenue code line item being denied (ten-position numeric field in 9999999.99 format) |
| FMR REASON-CODES | Identifies when a claim is edited in the system, based on a parameter in the Medical Policy Parameter file (five-position alphanumeric field with four occurrences) |
| ORIG | Original HCPC billed and modifiers billed (five-position alphanumeric HCPC and up to five two-position alphanumeric modifiers) |
| ORIG REV | Original revenue code billed (four-position numeric field) |
| MR | Identifies if the service received complex manual medical review (one-position alphanumeric field) Valid Values: Y ‒ Medical records received. This service received complex manual medical review. N ‒ Medical records were not received. This service received routine manual medical review. Blank ‒ The services did not receive manual medical review (default value). |
| ODC REASON-CODES | Original Denial Reason Codes ‒ only populated when there is a line user action code and a corresponding medical review denial reason code in the Benefits Savings portion of claim (five-position alphanumeric field with four occurrences) |
| OCE OVR | Identifies how the OCE module controls the overrides for the line item (one-position alphanumeric field) |
| CWF OVR | This field bypasses edit 5390 and does not generate alert code 7703 (one-position alphanumeric field) Valid Values: 1 ‒ Home Health consolidated billing 2 ‒ Skilled Nursing Facility consolidated billing T ‒ Therapy Override |
| NCD OVR | Identifies whether the line has been reviewed for medical necessity and should bypass the NCD edits, the line has no covered charges and should bypass the NCD edits, or the line should not bypass the NCD edits (one-position alphanumeric field) Valid Values: Y ‒ The line has been reviewed for medical necessity and bypasses the NCD edits. D ‒ The line has no covered charges and bypasses the NCD edits. Blank ‒ The NCD edits are not bypassed, (default value). Note: a blank in this field is set on all lines for resubmitted RTP claims. |
| NCD DOC | Identifies whether the documentation was received for the medically necessary service (one-position alphanumeric field) Valid Values: Y ‒ The documentation supporting the medical necessity was received. N ‒ The documentation supporting the medical necessity was not received, (default value.) |
| NCD RESP | Identifies the response code that is returned from the NCD edits (one-position alphanumeric field) Valid Values: 0 ‒ The HCPCS/Diagnosis code matched the NCD edit table pass criteria. The line continues through the system’s internal local medical necessity edits. 1 ‒ The line continues through the system’s internal local medical necessity edits, because the HCPCS code was not applicable to the NCD edit table process, the date of service was not within the range of the effective dates for the codes, the override indicator is set to Y or D, or the HCPCS code field is blank. 2 ‒ None of the diagnoses supported the medical necessity of the claim (list 3 codes), but the documentation indicator shows that the documentation to support medical necessity is provided. The line suspends for medical review. 3 ‒ The HCPCS/Diagnosis code matched the NCD edit table list ICD-9-CM deny codes (list 2 codes). The line suspends and indicates that the service is not covered and is to be denied as beneficiary liable due to noncoverage by statute. 4 ‒ None of the diagnosis codes on the claim support the medical necessity for the procedure (list 3 codes) and no additional documentation is provided. This line suspends as not medically necessary and will be denied. 5 ‒ Diagnosis codes were not passed to the NCD edit module for the NCD HCPCS code. The claim suspends and the FI will RTP the claim. Blank ‒ Set to space for all lines on resubmitted RTP'D claims, (default value.) |
| NCD# | Identifies the NCD number associated with the beneficiary’s claim denial (eight-position alphanumeric field) |
| OLUAC | Original Line User Action Code ‒ only populated when there is a line user action code and a corresponding medical review denial reason code in the Benefits Savings portion of claim (one-position alphanumeric field with four occurrences) |
| LUAC | Identifies the cause of denial for the revenue line and a reconsideration code. The denial code (1st position) must be present in the system and predefined in order to capture the correct denial reason. The values are equal to the values listed for User Action Codes. The reconsideration code (2nd position) has a value equal to R indicating to the system that a reconsideration has been performed (two-position alphanumeric field with four occurrences) Valid Values: 1 ‒ LUAC lines present 2 ‒ Non-LUAC lines present |
| NON COV-UNT | Number of days/visits that are being denied ‒ Denied days/visits are required for those revenue codes that require units on Revenue Code file (seven-position numeric field with four occurrences in 9999999 format) The first line occurrence of noncovered units on the revenue code line 0001 identifies the total non-covered units for all lines containing a LUAC on this screen. The second line occurrence of noncovered units on the revenue code line 0001 identifies the total noncovered units for all lines not containing a LUAC on this screen. |
| NON COV-CHRG | Total number of denied/rejected/noncovered charges for each line item being denied (ten-position numeric field with four occurrences in 9999999.99 format) The first line occurrence of noncovered charges on the revenue code line 0001 identifies the total noncovered charges for all lines containing a LUAC on this claim. The second line occurrence of non-covered charges on the revenue code line 0001 identifies the total noncovered charges for all lines not containing a LUAC on this screen. |
| DENIAL REAS | Cause Of Denial for the revenue code line. The denial code must be present in the system and predefined in order to capture the correct denial reason (five-position alphanumeric field with four occurrences) |
| OVER CODE | ANSI override code that allows the operator to manually override the system generated ANSI codes taken from the Denial Reason Code file (one-position alphanumeric field with four occurrences) |
| ST/LC OVER | Identifies the override of the reason code file status when a line item has been suspended (one-position alphanumeric field with four occurrences) |
| MED TEC | Medical Technical Denial indicator ‒ used when performing the medical review denial of a line item (one-position alphanumeric field with four occurrences) Valid Values: A ‒ Home Health only ‒ not intermittent care ‒ technical and waiver was applied B ‒ Home Health only ‒ not homebound ‒ technical and waiver was applied C ‒ Home Health only ‒ lack of physicians orders ‒ technical deletion and waiver was not applied D ‒ Home Health only ‒ Records not submitted after the request ‒ technical deletion and waiver was not applied M ‒ Medical denial and waiver was applied S ‒ Medical denial and waiver was not applied T ‒ Technical denial and waiver was applied U ‒ Technical denial and waiver was not applied |
| ANSI ADJ | ANSI Adjustment Reason Code ‒ data for this field is from the ANSI file housed as the second page in the Reason Code file. The ANSI codes that appear on the line item can be replaced with a new code and the system processes the denial with the entered code. The ANSI code is built off of the denial code used for each line item. Each denial code must be present on the Reason Code file to assign the ANSI code to the denial screen (three-position alphanumeric field with four occurrences) |
| ANSI GROUP | ANSI Group code ‒ data for this field is from the ANSI file housed as the second page in the Reason Code file. The ANSI codes that appear on the line item can be replaced with a new code and the system processes the denial with the entered code. The ANSI code is built off of the denial code used for each line item. Each denial code must be present on the reason code file to assign the ANSI code to the denial screen (two-position alphanumeric field with four occurrences) |
| ANSI REMARKS | ANSI Remarks codes ‒ data for this field is taken from the ANSI file housed as the second page in the Reason code file. The ANSI codes that appear on the line item can be replaced with a new code and the system processes the denial with the entered code. The ANSI code is built off of the denial code used for each line item. Each denial code must be present on the reason code file to assign the ANSI code to the denial screen (four-position alphanumeric field with a maximum of four occurrences on each of the four lines) |
| TOTAL | Total of all revenue code noncovered units and charges present on MAP171D (noncovered units is a seven-position numeric field in 9999999; noncovered charges is a nine-position numeric field in 9999999.99 format) |
| LINE ITEM REASON CODES | Reason code that is assigned out of the system for suspending the line item. There are four FISS reason codes that can be assigned to the line level (five-position alphanumeric field with four occurrences) |
Press the <F8/PF8> key to access Claim Page 03 to key reimbursement information.
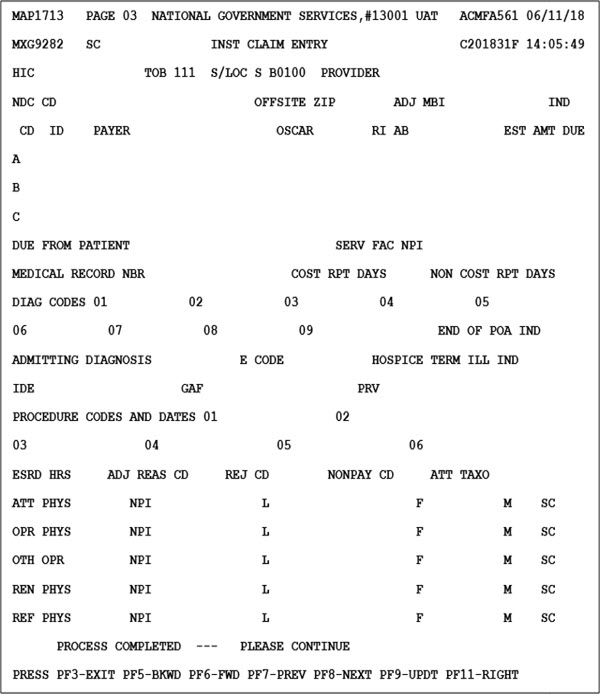
| Field | Description |
|---|---|
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Current status/location of claim |
| PROVIDER | Provider NPI (13-position alphanumeric field) |
| NDC CD | National Drug Code - used for the crossover Medicaid Drug Rebate data submitted on the UB04 paper claims and DDE claims (24-position alphanumeric field in the following sequence (left justified): Valid Values: Position 1–2 – N4 Qualifier Position 3–13 – National Drug Code Position 14–15 – Last two position of the National Drug Code (no delimiter) the Unit of Measurement Qualifier. Valid Values: F2 – International Unit GR – Gram ML – Milliliter UN – Unit |
| OFFSITE ZIP | Identifies offsite clinic/outpatient department ZIP Codes. It determines the claim line health professional shortage area (HPSA)/physician scarcity area (PSA) bonus eligibility, for both online and batch processing. (five-position alphanumeric field) Note: When a ZIP Code is present, the system uses the ZIP code for processing, not the ZIP code for the base provider (critical access hospital [CAH]). Indicating that one of the off-site clinics/outpatient departments submitted the claim for payment and not the base provider (CAH). |
| ADJ MBI | Identifies the MBI number submitted on the adjustment/cancel claim (11-position alphanumeric field) |
| IND | Identifies if the adjustment/cancel claim was submitted with a HIC or MBI number (one-position alphanumeric field) Valid Values: H – The HIC was submitted on the adjustment/cancel claim. M – The MBI was submitted on the adjustment/cancel claim. Blank – This field will be blank on adjustment/cancel claims created prior to 7/01/18 and non-adjustment/cancel claims. |
| CD | Identifies the specific payer code (one-position alphanumeric field with three occurrences) |
| ID | Payer Identification Number (five-position alphanumeric field with three occurrences) |
| PAYER | Payer name identifying each payer organization from which the provider might expect some payment for the claim (25-position alphanumeric field with three occurrences) Note: When a Z is entered as the payer code identifying Medicare as a payer, the payer name Medicare must be entered as well. |
| OSCAR | OSCARprovider number (13-position alphanumeric field with three occurrences) |
| RI | Release of Information – displays whether or not the provider has on file a signed statement permitting the provider to release data to other organizations in order to adjudicate the claim (one-position alphanumeric field with three occurrences) Valid Values: Y ‒ Yes R ‒ Restricted or modified release N ‒ No release |
| AB | Assignment of Benefits ‒ displays whether or not the provider has a signed form authorizing the third party payer to pay the provider (two-position alphanumeric field with three occurrences) Valid Values: Y ‒ Benefits assigned N ‒ No benefits assigned |
| EST AMT DUE | Amount estimated by the provider still due from the indicated payer ‒ estimated responsibility less prior payments (ten-position numeric field 9999999.99 format, and occurs three times) |
| DUE FROM PATIENT | Due from patient amount ‒ the amount the provider has received from the beneficiary toward payment of this claim prior to the billing date. Entry is required only in prior payments portion of this field (ten-position numeric field in 99999999.99 format) |
| SERV FAC NPI | Service facility location NPI number ‒ used to enter the facility NPI of where the services were provided when other than the billing provider (ten-position numeric field) |
| MEDICAL RECORD NBR | Number assigned to the patient’s medical/health record by the provider (17-position alphanumeric field) |
| COST RPT DAYS | Cost Report Days ‒ number of days claimable as Medicare patient days for inpatient and SNF types of bills (11X, 41X, 18X, 21X, 28X and 51X) on the cost report (three-position alphanumeric field). The system calculates this field and generates the applicable data. |
| NON COST RPT DAYS | Non-Cost Report Days ‒ number of days not claimable as Medicare patient days for inpatient and SNF types of bills (11X, 18X, 21X, 28X, 41X and 51X) on the cost report (three-position alphanumeric field) |
| DIAG CODES | Diagnosis codes ‒ ICD-10 code(s) describing the principal diagnosis (first code) and additional conditions (codes two through 25) that co-exist at the time of admission, or develop subsequently (seven-position alphanumeric field with nine occurrences) |
| END OF POA IND | End of POA indicator ‒ last character of the Present On Admission (POA) indicator, effective with discharges on or after 01/01/08 (one-position alphanumeric field) Valid Values: Z ‒ The end of POA indicators for principal and, if applicable, other diagnoses. X ‒ The end of POA indicators for principal and, if applicable, other diagnoses in special processing situations that may be identified by CMS in the future. Blank ‒ Not acute care, POAs do not apply. |
| ADMITTING DIAGNOSIS | Admitting Diagnosis ‒ diagnosis code describing the inpatient condition at the time of the admission (seven-position alphanumeric field) |
| E CODE | External Cause Code ‒ ICD-10 code for the external cause of an injury, poisoning, or adverse effect (seven-position alphanumeric field) |
| HOSPICE TERM ILL IND | Hospice Patient Terminal Illness Indicator ‒ whether or not a hospice patient has a terminal illness. It is only used for hospice claims (one-position alphanumeric field) Valid Values: Y ‒ The patient is terminal N ‒ The patient is not terminal |
| IDE | Investigational Device Exemption number ‒ IDE authorization number assigned by the FDA (15-position alphanumeric field) |
| GAF | Geographic Adjustment Factors for state, carrier and locality at the claim level (13-position numeric field in 999999999.99 format) |
| PRV | Patient Reason for Visit ‒ ICD-10-CM code describing the patient’s stated reason for seeking care at the time of outpatient registration (even-position alphanumeric field with three occurrences) |
| PROCEDURE CODES AND DATES | Procedure Codes ‒ principal procedure (first code) and other procedures (codes two through 25) performed during the billing period covered by this claim. This field is required for inpatient claims where a surgical procedure is performed (seven-position alphanumeric field with six occurrences) Procedure Code Date – date corresponding with the procedure code. This is the date on which the procedure was performed (six-position alphanumeric field in MMDDYY format with six occurrences) |
| ESRD HRS | End Stage Renal Disease (ESRD) hours ‒ number of hours of certain dialysis treatments such as peritoneal (two-position numeric field) |
| ADJ REAS CD | Adjustment Reason Code ‒ type of adjustment being performed (two-position alphanumeric field) |
| REJ CD | Reject Code ‒ reason code for which the claim is being non-medically denied (five-position alphanumeric field) |
| NONPAY CD | Non-pay code ‒ reason for Medicare’s decision not to make payment (two-position alphanumeric field) |
| ATT TAXO | Attending Physician Taxonomy Code (ten-position alphanumeric field) |
| ATT PHYS | Licensed Attending Physician’s Identification Number or UPIN Code (six-position alphanumeric field) |
| NPI | National Provider Identifier number (ten-position alphanumeric field) |
| L | Last Name of the attending physician (17-position alphanumeric field) |
| F | First Name of the attending physician (eight-position alphanumeric field) |
| M | Middle Initial of the attending physician (one-position alphanumeric field) |
| SC | Physician Specialty Code (two-position alphanumeric field) |
| OPR PHYS | Licensed Operating Physician’s Identification Number or UPIN Code (six-position alphanumeric field) |
| NPI | National Provider Identifier number (ten-position alphanumeric field) |
| L | Last Name of the attending physician (17-position alphanumeric field) |
| F | First Name of the attending physician (eight-position alphanumeric field) |
| M | Middle Initial of the attending physician (one-position alphanumeric field) |
| SC | Physician Specialty Code (two-position alphanumeric field) |
| OTH OPR | Licensed, Other Operating Physician’s Identification Number or UPIN Code (six-position alphanumeric field) |
| NPI | National Provider Identifier number (ten-position alphanumeric field) |
| L | Last Name of the attending physician (17-position alphanumeric field) |
| F | First Name of the attending physician (eight-position alphanumeric field) |
| M | Middle Initial of the attending physician (one-position alphanumeric field) |
| SC | Physician Specialty Code (two-position alphanumeric field) |
| REN PHYS | Licensed Rendering Physician’s Identification Number or UPIN Code (six-position alphanumeric field) |
| NPI | National Provider Identifier number (ten-position alphanumeric field) |
| L | Last Name of the attending physician (17-position alphanumeric field) |
| F | First Name of the attending physician (eight-position alphanumeric field) |
| M | Middle Initial of the attending physician (one-position alphanumeric field) |
| SC | Physician Specialty Code (two-position alphanumeric field) |
| REF PHYS | Licensed Referring Physician’s Identification Number or UPIN Code (six-position alphanumeric field) |
| NPI | National Provider Identifier number (ten-position alphanumeric field) |
| L | Last Name of the attending physician (17-position alphanumeric field) |
| F | First Name of the attending physician (eight-position alphanumeric field) |
| M | Middle Initial of the attending physician (one-position alphanumeric field) |
| SC | Physician Specialty Code (two-position alphanumeric field) |
Press the <F11/PF11> key to access Claim Page 03, First Right View to key in the appropriate payment information for up to two primary payers.
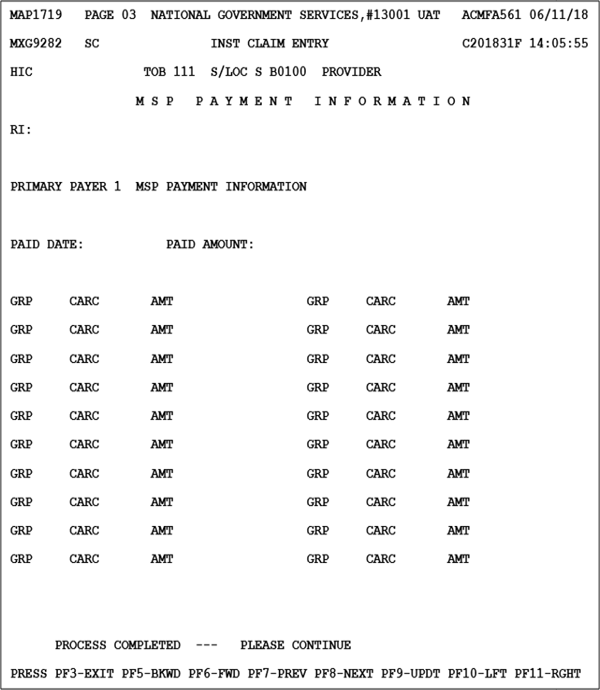
Press the <F11/PF11> key to access Claim Page 03 Second mRight View to enter the Provider Practice Location Address.
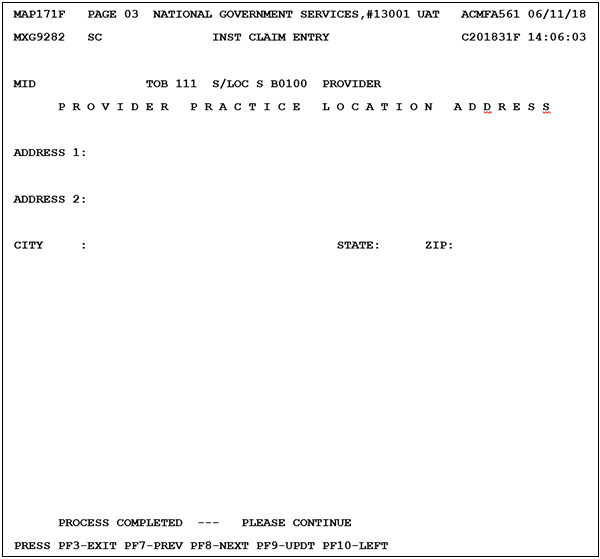
| Field | Description |
|---|---|
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Current status/location of claim |
| PROVIDER | Provider NPI (13-position alphanumeric field) |
| ADDRESS 1 | Service Facility Address 1 (55-position alphanumeric field) |
| ADDRESS 2 | Service Facility Address 2 (55-position alphanumeric field) |
| CITY | Service Facility City (30-position alphanumeric field) |
| STATE | Service Facility State (two-position alpha field) |
| ZIP | Service Facility ZIP (15-position numeric field) |
Press the <F11/PF11> key to access Claim Page 03 Third Right View to view QIES OASIS INFORMATION.
The purpose of this screen (MAP171G) is to display the OASIS information and make it viewable for Home Health providers.
Please note this is a view-only option. Details will be included once a claim has been submitted.
MAP171G includes the OASIS data returned from IQIES. MAP171G shows the OASIS item number and abbreviated description. The column labeled OA is the response that was sent from IQIES. The column labeled MR is for Medical Review. These fields are both protected and are for display purposes only.
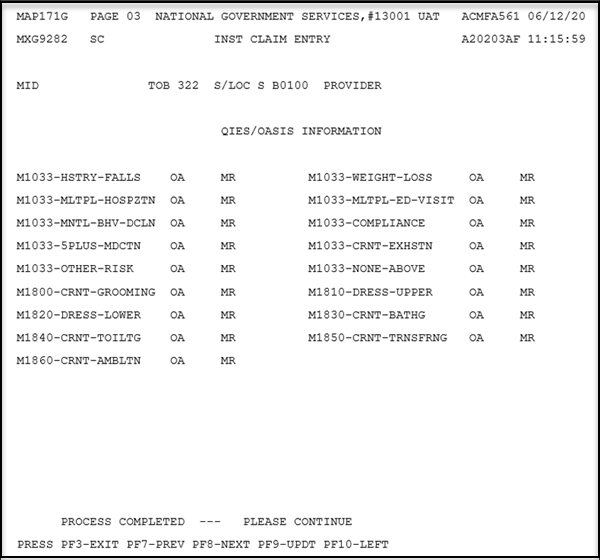
Valid Values:
00 – Able to get to and from the toilet and transfer independently with or without a device.
01 – When reminded, assisted, or supervised by another person, able to get to and from the toilet and transfer.
02 – Unable to get to and from the toilet but is able to use a bedside commode (with or without assistance).
03 – Unable to get to and from the toilet or bedside commode but is able to use a bedpan/urinal independently.
04 – Is totally dependent in toileting.
99 – No iQIES Assessment found
| Field | Description |
|---|---|
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Current status/location of claim |
| PROVIDER | Provider NPI (13-position alphanumeric field) |
| M1033-HSTRY-FALLS OA/MR | Indicates whether there are risk factors for hospitalization-falls (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-WEIGHT-LOSS OA/MR | Indicates whether there are risk factors for hospitalization-weight loss (one-position numeric field) either 0, 1 or 9. Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-MLTPL-HOSPZTN OA/MR | Indicates whether there are risk factors for hospitalization-multiple hospitalizations (one-position numeric field) either 0, 1 or 9. Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-MLTPL-ED-VISIT OA/MR | Indicates whether there are risk factors for hospitalization-multiple emergency department visitis (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-MNTL-BHV-DCLN OA/MR | Indicates whether there are risk factors for hospitalization-mental behavior decline (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-COMPLIANCE OA/MR | Indicates whether there are risk factors for hospitalization-compliance.Entries must be one-position numeric field)? Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-5PLUS-MDCTN OA/MR | Indicates whether there are risk factors for hospitalization-currently taking five or more medications (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-CRNT-EXHSTN OA/MR | Indicates whether there are risk factors for hospitalization-exhaustion (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-OTHER-RISK OA/MR | Indicates whether there are risk factors for hospitalization-other risks (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1033-NONE-ABOVE OA/MR | Indicates whether there are risk factors for hospitalization-none of the above (one-position numeric field) Valid Values: 0 – Unchecked (No) 1 – Checked (Yes) 9 – No iQIES Assessment found |
| M1800-CRNT-GROOMING OA/MR | Indicates Grooming: Current ability to tend safely to personal hygiene needs (specifically: washing face and hands, hair care, shaving or make up, teeth or denture care, or fingernail care) (two-position numeric field) Valid Values: 00 – Able to groom self unaided, with or without the use of assistive devices or adapted methods. 01 – Grooming utensils must be placed within reach before able to complete grooming activities. 02 – Someone must assist the patient to groom self. 03 – Patient depends entirely upon someone else for grooming needs. 99 – No iQIES Assessment found |
| M1810-DRESS-UPPER OA/MR | Indicates Current Ability to Dress Upper Body safely (with or without dressing aids) including undergarments, pullovers, front-opening shirts and blouses, managing zippers, buttons, and snaps (two-position numeric field) Valid Values: 00 – Able to get clothes out of closets and drawers, put them on and remove them from the upper body without assistance. 01 – Able to dress upper body without assistance if clothing is laid out or handed to the patient.02 – Someone must help the patient put on upper body clothing. 03 – Patient depends entirely upon another person to dress the upper body. 99 – No iQIES Assessment found |
| M1820-DRESS-LOWER OA/MR | Indicates Current Ability to Dress Lower Body safely (with or without dressing aids) including undergarments, slacks, socks or nylons, shoes (two-position numeric field) Valid Values: 00 – Able to obtain, put on, and remove clothing and shoes without assistance. 01 – Able to dress lower body without assistance if clothing and shoes are laid out or handed to the patient. 02 – Someone must help the patient put on undergarments, slacks, socks or nylons and shoes. 03 – Patient depends entirely upon another person to dress lower body. 99 – No iQIES Assessment found |
| M1830-CRNT-BATHG OA/MR | Indicates Bathing: Current ability to wash entire body safely. Excludes grooming (washing face, washing hands and shampooing hair) (two-position numeric field) Valid Values: 00 – Able to bathe self in shower or tub independently, including getting in and out of tub/shower. 01 – With the use of devices, is able to bathe self in shower or tub independently, including getting in and out of the tub/shower. 02 – Able to bathe in shower or tub with the intermittent assistance of another person:
03 – Able to participate in bathing self in shower or tub, but requires presence of another person throughout the bath for assistance or supervision. |
| M1840-CRNT-TOILTG OA/MR | Indicates Toilet Transferring: Current ability to get to and from the toilet or bedside commode safely and transfer on and off toilet/commode. (two-position numeric field) |
| M1850-CRNT-TRNSFRNG OA/MR | Indicates Transferring: Current ability to move safely from bed to chair, or ability to turn and position self in bed if patient is bedfast (two-position numeric field) Valid Values: 00 – Able to independently transfer. 01 – Able to transfer with minimal human assistance or with use of an assistive device. 02 – Able to bear weight and pivot during the transfer process but unable to transfer self. 03 – Unable to transfer self and is unable to bear weight or pivot when transferred by another person. 04 – Bedfast, unable to transfer but is able to turn and position self in bed. 05 – Bedfast, unable to transfer and is unable to turn and position self. 99 – No iQIES Assessment found |
| M1860-CRNT-AMBLTN OA/MR | Indicates Ambulation/Locomotion: Current ability to walk safely, once in a standing position, or use a wheelchair, once in a seated position, on a variety of surfaces. (two-position numeric field) Valid Values: 00 – Able to independently walk on even and uneven surfaces and negotiate stairs with or without railings (specifically: needs no human assistance or assistive device). 01 – With the use of a one-handed device (for example, cane, single crutch, hemi-walker), able to independently walk on even and uneven surfaces and negotiate stairs with or without railings. 02 – Requires use of a two-handed device (for example, walker or crutches) to walk alone on a level surface and/or requires human supervision or assistance to negotiate stairs or steps or uneven surfaces. 03 – Able to walk only with the supervision or assistance of another person at all times. 04 – Chairfast, unable to ambulate but is able to wheel self independently. 05 – Chairfast, unable to ambulate and is unable to wheel self. 06 – Bedfast, unable to ambulate or be up in a chair. 99 – No iQIES Assessment found |
Press the <F8/PF8> key to access Claim Page 04 to enter Remarks.
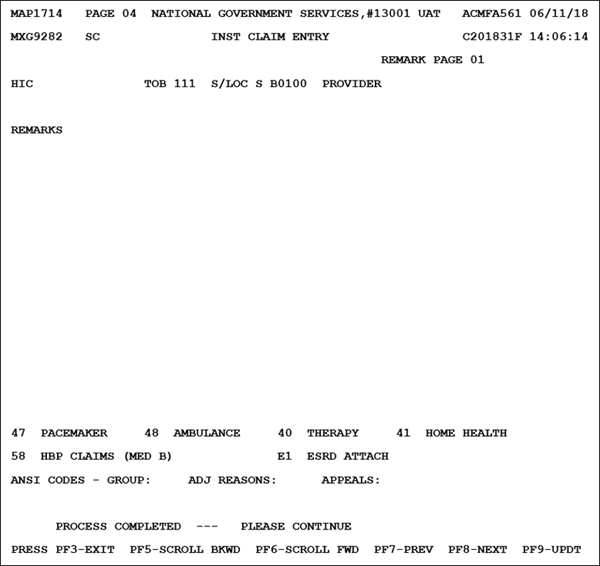
| Field | Description |
|---|---|
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Current status/location of claim |
| PROVIDER | Provider NPI (13-position alphanumeric field) |
| ZIP | ZIP code for Hardcopy/EMC in the following format: ZIP Code (five-position alphanumeric) Carrier (five-position alphanumeric) Locality (two-position alphanumeric) Rural Indicator (one-position alphanumeric) State (two-position alpha) Rural Indicator 2 (one-position alphanumeric) Year Quarter (five-position alphanumeric) |
| REMARKS | Remarks information as submitted on automated claims, as well as provide internal staff with a mechanism to provide permanent comments regarding special considerations that played a part in adjudicating the claim. Example: The Medical Review Department may use this area to document their rationale for the final medical determination or to provide additional information to the Waiver Employee to assist that individual with claim finalization. The remarks field is also used for providers to furnish justification for late filed claims that override the intermediary’s existing reason code for timeliness. The following information must be entered on the first line. Additional information may be entered on the second and subsequent lines of the remarks section for further justification. Select one of the following reasons and enter the information exactly as it appears below: Justify: MSP involvement Justify: SSA involvement Justify: PRO Review involved Justify: Other involvement Additional Remarks space is available by using the <F6/PF6> key to scroll forward (78-position alphanumeric field with ten occurrences) |
| 47 PACEMAKER, 48 AMBULANCE, 40 THERAPY, 41 HOME HEALTH, 58 HBP CLAIMS, (MED B), E1 ESRD ATTACH | Attachment records associated with the claim. Attachment records are additional required documents that are submitted by the provider attached to a claim. The system considers these part of the claim record either after manual entry or system generation of the information (two-position alphanumeric field) By utilizing the SC field and inserting the number of the appropriate attachment to be entered, the system provides the appropriate entry screen. The attachment selections are: 47 ‒ Pacemaker 48 ‒ Ambulance 40 ‒ Therapy screens (physical, speech, cardiac rehab, occupational, pulmonary rehab and inhalation) 41 ‒ Home Health 58 ‒ Hospital Based Physician Claims E1 ‒ ESRD Attach |
| ANSI CODES-GROUP | General Category Of Payment Adjustment ‒ used for claims submitted in an ANSI automated format only (two-position alphanumeric field) |
| ADJ REASONS | Claim Adjustment Standard Reason Code identifying the detailed reason the adjustment was made (three-position alphanumeric field). See Claim Page 03 for values. |
| APPEALS | ANSI Appeal Codes for inpatient or outpatient (five-position alphanumeric field with three occurrences) |
After keying Remarks, press the <F8/PF8> key to access Claim Page 05.
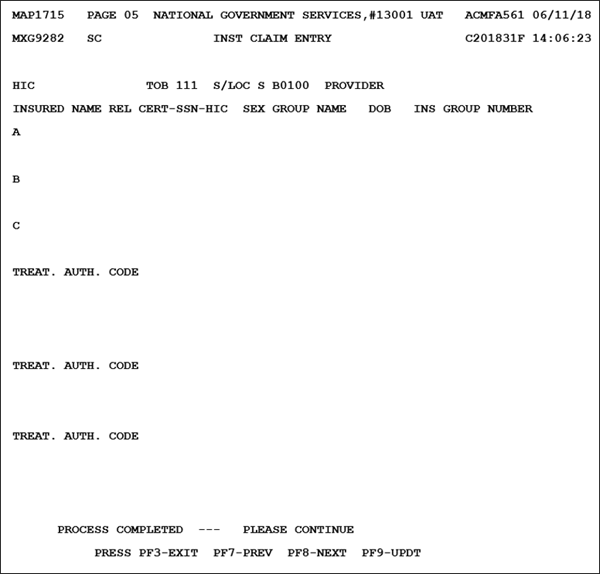
| Field | Description |
|---|---|
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Current status/location of claim |
| PROVIDER | Provider NPI (13-position alphanumeric field) |
| INSURED NAME | Insured name – Identifies the individual in whose name the insurance is carried, as qualified by the payer organization (ten-position alphanumeric field for the first name; 15-position field for the last name). Note: Insured Name must be the same as on the patient’s health insurance card or other Medicare notice. If billing supplemental insurance, enter the name of the individual insured under Medicare line A and enter the name of the individual insured under a supplemental policy on line B. Complete this section by entering the name of the individual in whose name the insurance is carried if there are payer(s) of higher priority than Medicare and the provider is requesting payment because: another payer paid some of the charges and Medicare is secondarily liable for the remainder; another payer denied the claim; or the provider is requesting conditional payment. |
| REL | Patient’s relationship to insured. On the same lettered line (A, B or C) that corresponds to the line which Medicare payer information is reported, enter code indicating relationship between the patient and the identified insured (two-position alphanumeric field with three occurrences). The codes listed in the following table are for Medicare requirements only. Other payers may require codes not reflected. |
| CERT-SSN-MID-ID NUMBER | Certification – Social Security Number–Medicare ID number–Identifies the insurer assigned beneficiary number or Medicare Beneficiary ID Number used in all correspondence and to facilitate the payment of claims (19-position alphanumeric field) |
| SEX | Identifies the sex of the beneficiary/patient (one-position alpha field) Valid values F = Female M = Male U = Unknown |
| GROUP NAME | Group name – Identifies the name of the group or plan through which the insurance is provided to the insured (18-position alphanumeric field |
| DOB | Date of birth – Identifies the insured’s date of birth (eight-position field in MMDDCCYY format) |
| INS GROUP NUMBER | Insurance group number – Displays the identification number, control number, or code assigned by the carrier or administrator to identify the group under which the individual is covered (20-position alphanumeric field) |
| TREAT AUTH CODE | HHPPS treatment authorization code – Identifies a matching key to the Outcome Assessment Information Set (OASIS) of the patient (18 positions with two eight-position dates (MMDDCCYYMMDDCCYY) followed by a two-position code (01‒10). The first date comes from M0030 that is the start of care date; the second date is from M0090 that is the date assessment completed. The codes are from M0100 that is for the assessment currently being completed for the following reasons: 01 = Start of care – further visits planned 02 = Start of care – no further visits planned 03 = Resumption of care (after inpatient stay) 04 = Rectification (follow-up) reassessment 05 = Other follow-up 06 = Transferred to an inpatient facility – patient not discharged from agency 07 = Transferred to an inpatient facility – patient discharged from agency 08 = Death at home 09 = Discharge from agency 10 = Discharge from agency – no visits completed after start/resumption of care assessment This field is also used to identify a Centers for Excellence or Provider Partnership Demonstration for NOA type of bill 11A and 11D. Valid values 07 = Centers for Excellence 08 = Providers Partnership Demonstration 09 – Discharge from agency 10 – Discharge from agency – no visits completed after start/resumption of care assessment |
Use the <F8/PF8> key to access Claim Page 06 to enter MSP Additional Insurer information.
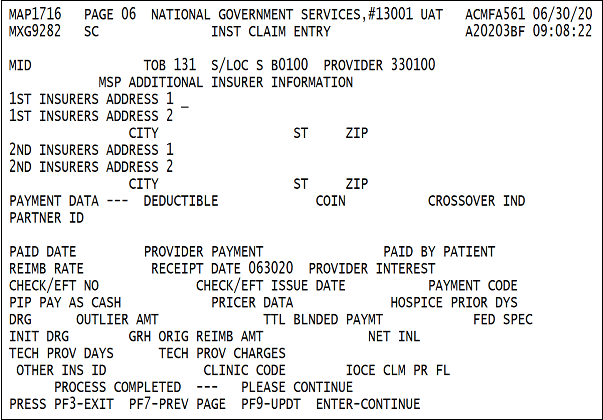
| Field | Description |
|---|---|
| MID | Medicare ID Number (system generated from Claim Page 01) |
| TOB | Type of bill (system generated from Claim Page 01) |
| S/LOC | Current status/location of claim |
| PROVIDER | Provider NPI (13-position alphanumeric field) |
| 1ST INSURERS ADDRESS 1 | 1st insurer’s address 1 –Identifies the street address of the beneficiary’s insurer (32-position alphanumeric field) |
| 1ST INSURERS ADDRESS 2 | 1st insurer’s address 2 – Identifies the second street address line of the beneficiary’s insurer and is used to indicate the P.O. box, apartment number, etc. (32-position alphanumeric field) |
| CITY | 1st insurer’s City – Identifies the insurer’s city address (15-position alphanumeric field) |
| ST | 1st insurer’s State – Identifies the insurer’s state address abbreviation. This must be a valid state abbreviation accepted by the U.S. Postal Service (two-position alphanumeric field) |
| ZIP | 1st insurer’s ZIP – Identifies the first five and then four positions of the insurer's ZIP code. |
| 2ND INSURERS ADDRESS 1 | 2nd insurer’s address 1 – Identifies the street address of the beneficiary’s insurer (32-position alphanumeric field) |
| 2ND INSURERS ADDRESS 2 | 2nd insurer’s address 2 – Identifies the second street address line of the beneficiary’s insurer and is used to indicate the P.O. box, apartment number, etc. (32-position alphanumeric field) |
| CITY | 2nd insurer’s City – Identifies the insurer’s city address (15-position alphanumeric field) |
| ST | 2nd insurer’s State – Identifies the insurer’s state address abbreviation. This must be a valid state abbreviation accepted by the U.S. Postal Service (two-position alphanumeric field) |
| ZIP | 2nd insurer’s ZIP – Identifies the first five and then four positions of the insurer's ZIP code |
| DEDUCTIBLE | Amount of Deductible for which the beneficiary/patient is liable. When the claim has processed to finalization, this field is system generated (ten-position numeric field in 9999999.99 format) |
| COIN | Amount of Coinsurance for which the beneficiary/patient is responsible. When the claim has processed to finalization, this field is system generated (eight-position numeric field in 99999.99 format) |
| CROSSOVER IND | Crossover Indicator – identifies the Medicare payor on the claim for payment evaluation of claims crossed over to their insurer's to coordinate benefits (one-position alphanumeric field) Valid Values: 1 – Primary 2 – Secondary 3 – Tertiary |
| PARTNER ID | Partner Identification Number (nine-position alphanumeric field with 10 occurrences) Also identifies the production COBA Trading Partner(s) that did not receive the claim due to claim errors (one-position alphanumeric that immediately follows each Partner ID) Valid Values: N – Not crossed over due to claim data errors Blank – Crossed Over |
| PAID DATE | Scheduled Payment Date of the claim or the date the provider is actually reimbursed (six-position numeric field in MMDDYY format) |
| PROVIDER PAYMENT | Provider Payment Amount (13-position alphanumeric field in 999999999.99- format) |
| PAID BY PATIENT | This field is not used by FISS |
| REIMB RATE | Per Diem Amount to be paid for an individual claim for those providers reimbursed on per diem reimbursement or percentage of reimbursement if the provider's type of reimbursement is based on a percentage of charges (six-position numeric field in 999.99 format) |
| RECEIPT DATE | Date the Claim was Received by the MAC (six-position numeric field in MMDDYY format) |
| PROVIDER INTEREST | Amount of Interest Paid to the Provider for late payment on clean claims (12-position numeric field in 999999999.99 format) |
| CHECKEFT NO | Identification number of the check or electronic funds transfer (ten-position alphanumeric field) |
| CHECK/EFT ISSUE DATE | Date the Check was Issued or the date the electronic funds transfer occurred (six-position numeric field in MMDDYY format) |
| PAYMENT CODE | Payment Method of the check or electronic funds transfer (three-position alphanumeric field) Valid Values: ACH – Automated Clearing House or Electronic Funds Transfer CHK – Check NON – Nonpayment Data |
| HOSPICE PRIOR DYS | Hospice prior period days provided by the CWF |
| DRG | Diagnosis Related Group code assigned by the CMS grouper program using length of stay, covered days, sex, age, diagnosis and procedure codes, discharge date and total charges (three-position alphanumeric field) |
| OUTLIER AMT | Outlier Portion of the PPS payment for capital and the PPS dollar threshold for a cost outlier (11-position numeric field in 99999999.99 format) |
| TTL BLENDED PAYMENT | TTL Blended Payment. This field is not used by FISS. |
| FED SPEC | This field is not used by FISS. |
| INIT DRG | Initial Diagnosis Related Group code assigned by the CMS grouper program using length of stay, covered days, sex, age, diagnosis and procedure codes, discharge date, and total charges. This additional MS-DRG field will allow the systems to pass on the initial MS-DRG in the event a HAC. impacts the final MS-DRG assignment (four-position numeric field) |
| GRH ORIG REIMB AMT | Amount Reduced from the Provider's Reimbursement as mandated by Gramm/Rudman/Hollings legislation (10-position numeric field in 999999.99- format) Note: For Inpatient Rehabilitation Facility (IRF) PPS claims, the IRF PPS pricer populates this field if a late assessment penalty has been applied to the claim. If present, the field contains the dollar amount of the penalty applied. |
| NET INL | This field is used in DDE. |
| TECH PROV DAYS | Days Present on the Benefit Savings Record or the days reflected in the occurrence span 77 if the benefit savings record is not present (three-position numeric field) |
| TECH PROV CHARGES | Technical Provider Liable charges present on the benefit savings record (ten-position numeric field in 9999999.99 format) |
| OTHER INS ID | This field not used by FISS. |
| CLINIC CODE | This field is not used by FISS. |
| IOCE CLM PR FL | Identifies the IOCE Claim Processed Flag (one-position numeric field with valid values 0, 1, 2, 3, 4, or 9) |
This is the last claim page to enter data. Use the <F7/PF7> and <F8/PF8> keys to review claim page details. Press the <F9/PF9> key to save and submit the claim.
If there are no errors, the claim is submitted. It disappears from the screen, and the next claim can be entered.
If there is an error, the reason code will appear in the lower-left corner of the screen.
- Press the <F1/PF1> key to access the reason code narrative. Review the narrative to determine the claim data elements that need to be corrected before claim submission.
- Press the <F3/PF3> key to return to the claim. Make the necessary claim element corrections, then press the <F9/PF9> key to update and resubmit the claim.
FISS/DDE Claim Page/UB-04 Locator Cross-Reference
Clam Page 01
| Data Entry Field Name | UB-04 Cross Reference |
|---|---|
| MID | Locator 60 A, B, C |
| TOB | Locator 4 |
| S/LOC | No crosswalk |
| OSCAR | Locator 51 |
| UB-FORM | No crosswalk |
| NPI | Locator 56 |
| TRANSFERING HOSPICE PROVIDER | No crosswalk |
| PROCESS NEW MID | Locator 60 A, B, C |
| PATIENT CONTROL NBR | Locator 3A |
| FED. TAX NO. | Locator 5 |
| TAX SUB: | Locator 5 |
| STMT DATES FROM | Locator 6 |
| TO | Locator 6 |
| DAYS COV | Substitute VC 80 |
| N-C | Substitute VC 81 |
| CO | Substitute VC 82 |
| LTR | Substitute VC 83 |
| LAST | Locator 08 |
| FIRST | Locator 08 |
| MI | Locator 08 |
| STREET | Locator 09 |
| CITY | Locator 09 |
| STATE | Locator 09 |
| ZIP | Locator 09 |
| DOB | Locator 10 |
| SEX | Locator 11 |
| MS | Eliminated |
| ADM DATE | Locator 12 |
| HOUR | Locator 13 |
| TYPE | Locator 14 |
| SRC | Locator 15 |
| D HR | Locator 16 |
| STAT | Locator 17 |
| MEDICAL RECORD NBR | Locator 3B |
| COST RPT DAYS | No crosswalk |
| NON COST RPT DAYS | No crosswalk |
| COND CODES | Locator 18‒28 |
| OCC CDS/DATE | Locator 31‒34A, B |
| OCCURRENCE SPAN AND DATE | Locator 35‒36 A, B |
| DCN | Locator 64 |
| VALUE CODES AND AMOUNTS | Locator 39‒41 A, B, C, D |
Claim Page 02
| Data Entry Field Name | UB-04 Cross Reference |
|---|---|
| MID | Locator 60 A, B, C |
| TOB | Locator 4 |
| S/LOC | No crosswalk |
| PROVIDER | Locator 51 |
| REV | Locator 42 |
| HCPC | Locator 44 |
| MODIFS | No crosswalk |
| TOT UNT | Locator 46 |
| COV UNT | Locator 46 |
| TOT CHARGE | Locator 47 |
| NCOV CHARGE | Locator 48 |
| SERV DT | Locator 45 |
Claim Page 03
| Data Entry Field Name | UB-04 Cross Reference |
|---|---|
| MID | Locator 60 A, B, C |
| TOB | Locator 4 |
| S/LOC | No crosswalk |
| OFFSITE ZIPCD | No crosswalk |
| PROVIDER | Locator 51 A, B, C |
| CD | Locator 50 A, B, C |
| ID | No crosswalk |
| PAYER | Locator 50 A, B, C |
| OSCAR | Locator 60 A, B, C |
| RI | Locator 52 A, B, C |
| AB | Locator 53 A, B, C |
| PRIOR PAY | Locator 54 A, B, C |
| EST AMT DUE | Locator 55 A, B, C |
| DUE FROM PATIENT | Eliminated |
| DIAGNOSIS CODES | Locator 67‒75 |
| ADMITTING DIAGNOSIS | Locator 69 |
| E CODE | Locator 77 |
| HOSPICE TERM ILL IND | No crosswalk |
| PROCEDURE CODES AND DATES | Locator 74a‒e |
| ESRD HOURS | No crosswalk |
| ADJUSTMENT REASON CODE | No crosswalk |
| REJECT CODE | No crosswalk |
| NON-PAY CODE | No crosswalk |
| ATTENDING NPI/QUAL/ID | Locator 76 |
| OPERATING NPI/QUAL/ID | Locator 77 |
| OTHER NPI/QUAL/ID | Locator 78 |
| NPI | Locator 56 |
Claim Page 04:
| Data Entry Field Name | UB-04 Cross Reference |
|---|---|
| MID | Locator 60 A, B, C |
| TOB | Locator 4 |
| S/LOC | No crosswalk |
| PROVIDER | Locator 51 A, B, C |
| REMARKS | Locator 80 |
Claim Page 05
| Data Entry Field Name | UB-04 Cross Reference |
|---|---|
| MID | Locator 60 A, B, C |
| TOB | Locator 4 |
| S/LOC | No crosswalk |
| PROVIDER | Locator 51 A, B, C |
| INSURED NAME | Locator 58 A, B, C |
| REL | Locator 59 A, B |
| CERT.-SSN-MID-ID | Locator 60 A, B, C |
| GROUP NAME | Locator 61 A, B, C |
| INS GROUP NUMBER | Locator 62 A, B, C |
| TREAT. AUTH. CODE 1, 2, 3 | Locator 63 A, B, C |
Claim Page 06
| Data Entry Field Name | UB-04 Cross Reference |
|---|---|
| MID | Locator 60 A, B, C |
| TOB | Locator 4 |
| S/LOC | No crosswalk |
| PROVIDER | Locator 51 A, B, C |
| 1ST INSUREDS ADDRESS 1, 2 | No crosswalk |
| CITY 1, 2 | No crosswalk |
| ST 1, 2 | No crosswalk |
| ZIP 1, 2 | No crosswalk |
| 2ND INSUREDS ADDRESS 1, 2 | No crosswalk |
Revised 4/11/2024