- Introduction
- Chapter I - Online System Terminology
- Chapter II - Online Menu Functions Overview
- Chapter III - Navigating the Online System
-
Chapter IV - Inquiries Submenu (01)
- Accessing the Inquiries Submenu
- Beneficiary/CWF (10)
- DRG (Pricer/Grouper) (11)
- Claim Summary (12)
- Revenue Codes (13)
- HCPCS Codes (14)
- DX/Proc Codes ICD-9 (15)
- Adjustment Reason Codes (16)
- Reason Codes (17)
- ZIP Code File (19)
- OSC Repository Inquiry (1A)
- Claim Count Summary (56)
- Home Health Payment Totals (67)
- ANSI Reason Codes (68)
- Invoice Number/DCN Translator (88)
- DX Proc Codes ICD-10 (1B)
- Community Mental Health Centers Services Payment Totals (1C)
- Check History (FI)
- Provider Practice Address Query (1D)
- New HCPCS Screen (1E)
- Opioid Use Disorder (OUD) Demo 99 (1F)
- Chapter V - Claims and Attachments Submenu (02)
- Chapter VI - Claims Correction Submenu (03)
- Chapter VII - Online Reports View Submenu (04)
-
Resources
- Part A Electronic Medicare Secondary and Tertiary Payer Specifications for ANSI Inbound Claim
- Electronic Medicare Secondary Payer Specifications for Inbound Claims
- FISS UB-04 Data Entry Payer Codes
- Common Claim Status/Locations
- FISS Reason Code Overview
- FISS Reason Code/Claim Driver Overview
- Program Function/Escape Key Crosswalk
- How to Adjust a Claim
- FISS Claim Change/Condition Reason Codes
- How to Cancel a Claim
- How to Correct a Return to Provider Claim
- Online System Menu Quick-Reference
Chapter IV: Inquiries Submenu (01)
OSC Repository Inquiry (1A)
Purpose
An occurrence span code identifies a specific event that relates to the payment of the claim that spans several days. The dates identify the commencement and ending of the event. Up to ten occurrence span codes may be reported on each claim.
The purpose of the OSC REPOSITORY INQUIRY screen is to display the claim’s occurrence span code repository record.
To access the OSC REPOSITORY INQUIRY option from the FISS online INQUIRIES submenu, type ‘1A’ at the Enter Menu Selection: prompt and press the <Enter> key.
Upon selecting the OSC REPOSITORY INQUIRY option, the DDE OSC REPOSITORY INQUIRY screen is available:
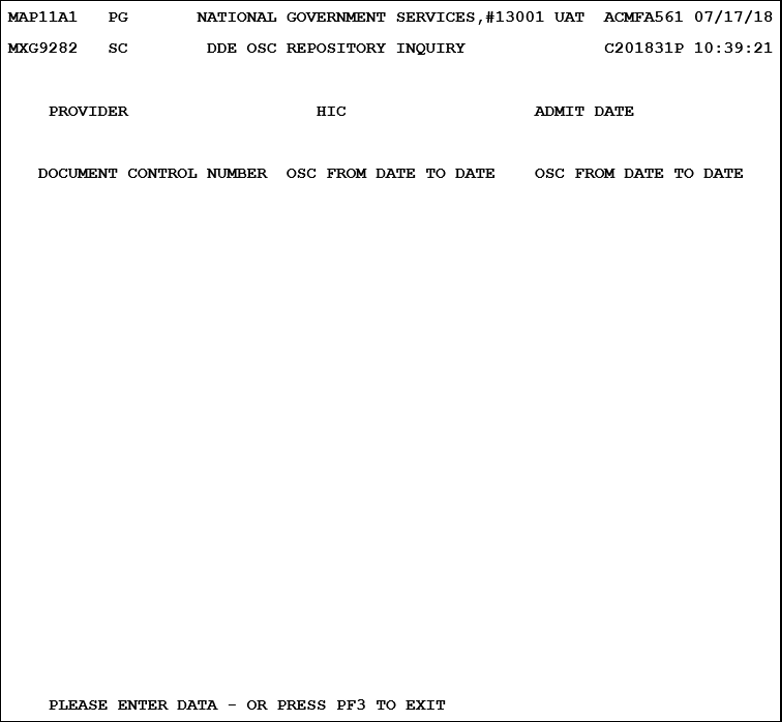
| Field | Description |
|---|---|
| Provider | Provider number ‑ identification number of the provider who is signed on |
| HIC | Medicare beneficiary number (12-position alphanumeric field) |
| ADMIT DATE | Patient’s Admission Date (a six-digit field in MMDDYY format) |
| DOCUMENT CONTROL NUMBER | Document Control Number ‑ identifies the DCN for a claim (23-position alphanumeric field) |
| OSC | Occurrence Span Code ‑ identifies events that relate to the payment of the claim. This is a two-position alphanumeric field. |
| FROM DATE | The occurrence span “from” date identifies the commencement date of the event that relates to the payment of a claim (eight-digit formatted date field in MMDDCCYY format) |
| TO DATE | The occurrence span “to” date identifies the ending date of the event that relates to the payment of a claim (eight-digit formatted date field in MMDDCCYY format) |
To access the OSC details from a specific claim, enter the beneficiary Medicare number in the HIC field and the date of admission in the ADMIT DATE field, then press the <Enter> key.
Occurrence Span Codes
| Code | Title | Description |
|---|---|---|
| M0 | QIO/UR Stay Dates | Partial approval – claim reviewed by PRO; some portion denied. Identifies the approved billing period |
| M1 | Provider Liability - No Utilization | Identifies a period of noncovered care that is denied due to lack of medical necessity or as custodial care for which the provider is liable. The beneficiary is not charged with utilization. The provider may not collect Part A or Part B deductible or coinsurance from the beneficiary. |
| M2 | Dates of Inpatient Respite Care | Identifies a period of inpatient respite care for hospice patients. |
| M3 | ICF Level of Care | Identifies a period of intermediate level of care during an inpatient hospital stay. |
| M4 | Residential Level of Care | Identifies a period of residential level of care during an inpatient stay. |
| M5‑MQ | - | Reserved for assignment by the NUBC |
| MR | - | Reserved for disaster related occurrence span code |
| MS | - | Reserved for assignment by the NUBC |
| 70 | Qualifying Stay Dates | Identifies a hospital stay of at least three days which qualifies the patient for payment of the SNF level of care services billed on this claim. (Part A claims for SNF level of care only.) |
| 70 | Nonutilization Dates (for payer use on hospital bills only) | A period of time during a PPS inlier stay for which the beneficiary had exhausted all regular days and/or coinsurance days, but which is covered on the cost report. |
| 71 | Prior Stay Dates | Identifies dates given by the patient for any hospital stay that ended within 60 days of this hospital or SNF admission. (Part A claims only.) |
| 72 | First/Last Visit | Identifies the first and last visits occurring in this billing period where these dates are different from the Statement Covers Period. |
| 74 | Noncovered Level of Care | Identifies repetitive Part B services to show a period of inpatient hospital care or of outpatient surgery during the billing period. |
| 75 | SNF Level of Care | Identifies a period of SNF level of care during an inpatient hospital stay. Since PRO’s no longer routinely review inpatient hospital bills for hospitals under PPS, this code is needed only in length of stay outlier cases. It is not applicable to swing-bed hospitals which transfer patients from the hospital to a SNF level of care. |
| 76 | Patient Liability | Identifies a period of noncovered care for which the hospital is permitted to charge the beneficiary. Code is to be used only where you or the PRO approve such charges in advance and the patient is notified in writing three days prior to the “From” date of this period. |
| 77 | Provider Liability – utilization charged | Identifies a period of noncovered care for which the provider is liable (other than for lack of medical necessity or as custodial care.) The beneficiary’s record is charged with Part A days, Part A or Part B deductible, and Part B coinsurance. The provider may collect Part A or Part B deductible and coinsurance from the beneficiary. |
| 78 | SNF Prior Stay Dates | Identifies a SNF stay that ended within 60 days of this hospital or SNF admission. An inpatient stay in a facility or part of a facility that is certified or licensed by the State solely below a SNF level of care does not continue a spell of illness. (Part A claims only.) |
| 79 | Verified Noncovered Stay Dates for Which the Provider is Liable | Verified noncovered stay dates for which the provider is liable |
| 80 | Prior same SNF Stay Dates for Payment Ban Purposes | Identifies a prior same-SNF stay indicating a patient resided in the SNF prior to, and if applicable, during a payment ban period up until their discharge to a hospital. |
Revised 8/16/2023