- Introduction
- Chapter I - Online System Terminology
- Chapter II - Online Menu Functions Overview
- Chapter III - Navigating the Online System
-
Chapter IV - Inquiries Submenu (01)
- Accessing the Inquiries Submenu
- Beneficiary/CWF (10)
- DRG (Pricer/Grouper) (11)
- Claim Summary (12)
- Revenue Codes (13)
- HCPCS Codes (14)
- DX/Proc Codes ICD-9 (15)
- Adjustment Reason Codes (16)
- Reason Codes (17)
- ZIP Code File (19)
- OSC Repository Inquiry (1A)
- Claim Count Summary (56)
- Home Health Payment Totals (67)
- ANSI Reason Codes (68)
- Invoice Number/DCN Translator (88)
- DX Proc Codes ICD-10 (1B)
- Community Mental Health Centers Services Payment Totals (1C)
- Check History (FI)
- Provider Practice Address Query (1D)
- New HCPCS Screen (1E)
- Opioid Use Disorder (OUD) Demo 99 (1F)
- Chapter V - Claims and Attachments Submenu (02)
- Chapter VI - Claims Correction Submenu (03)
- Chapter VII - Online Reports View Submenu (04)
-
Resources
- Part A Electronic Medicare Secondary and Tertiary Payer Specifications for ANSI Inbound Claim
- Electronic Medicare Secondary Payer Specifications for Inbound Claims
- FISS UB-04 Data Entry Payer Codes
- Common Claim Status/Locations
- FISS Reason Code Overview
- FISS Reason Code/Claim Driver Overview
- Program Function/Escape Key Crosswalk
- How to Adjust a Claim
- FISS Claim Change/Condition Reason Codes
- How to Cancel a Claim
- How to Correct a Return to Provider Claim
- Online System Menu Quick-Reference
Chapter IV: Inquiries Submenu (01)
Reason Codes (17)
Purpose
FISS reason codes are five-digit alphanumeric codes that indicate the outcome of claim editing and processing.
The REASON CODE option provides details to indicate why the claim met its disposition. In cases where the claim has been RTPd, rejected or denied the reason code narrative provides instructions on how to resolve the claim issue(s).
This option provides information on claim- and line-level reason codes without needing to access a specific claim.
To access the REASON CODES option from the FISS online INQUIRIES submenu, type ‘17’ at the Enter Menu Selection: prompt and press the <Enter> key.
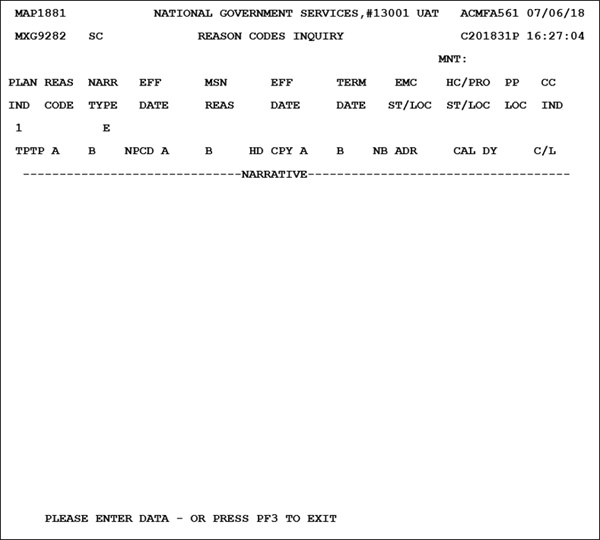
Upon selecting the REASON CODES option, the initial REASON CODES INQUIRY screen is available:
To review the narrative information for a specific reason code, type the five-digit reason code in the REAS CODE field, then press the <Enter> key.
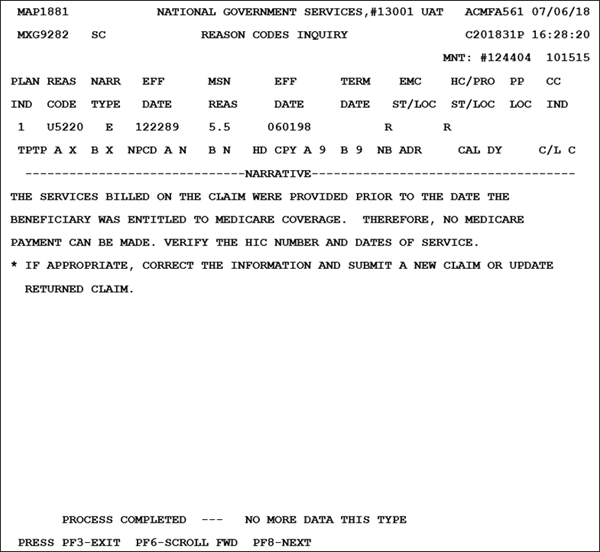
In the example included below, Reason Code U5220 is displayed:
| Field | Description |
|---|---|
| PLAN IND | Plan indicator – One-position alphanumeric field. Default = ‘1’ |
| REAS CODE | Reason code – Five-digit alphanumeric reason code |
| NARR TYPE | Narrative type – identifies whether the message is the standard, internal, or external message. This field defaults to the ‘E’ for external message for DDE providers (one-position alphabetic field) |
| EFF DATE | Identifies an effective date for the reason code or condition (six-position numeric field, MMDDYY format) |
| MSN REAS | Medicare Summary Notice Reason – used when MSNs are produced condition (six-position numeric field, MMDDYY format) |
| EFF DATE | Effective date for the alternate MSN reason code condition (six-position numeric field, MMDDYY format) |
| TERM DATE | Termination date for the alternate MSN reason code condition (six-position numeric field, MMDDYY format) |
| EMC ST/LOC | Electronic media claims status and location – Identifies the status and the location to be set on an automatic claim when it encounters the condition for a particular reason code. The first-alphanumeric position represents the status of the claim. The next five-alphanumeric positions represent the location. |
| HC/PRO S/LOC | Hardcopy/peer review organization status/location – Identifies the status and the location to be set on a hardcopy or a peer review organization (PRO) claim when it encounters the condition for a particular reason code. The first-alphanumeric position represents the status of the claim. The next five-alphanumeric positions represent the location. |
| PP LOC | Postpay location – Identifies the five-position alphanumeric postpay location of B75XX if the reason code is to send a claim to the postpay driver for postpay developmental activities. |
| CC IND | Clean claim indicator – The clean claim indicator instructs the system whether or not to pay interest if applicable. Valid values: A = PIP other B = PIP clean C = Non-PIP other D = Non-PIP clean E = Additional information was requested (non-PIP reimbursement) F = Additional information was requested (PIP reimbursement) G = A reply has been received from CWF providing a date of death. The date of death is prior to or overlaps the dates of service on the claim; therefore, development was required in order to process the claim (non-PIP reimbursement) H = A reply has been revived from the CWF providing a date of death. The date of death is prior to or overlaps the dates of service on the claim; therefore, development was required in order to process the claim (PIP reimbursement) I = A nondefinitive response was received from the CWF requiring development (non-PIP reimbursement) J = A nondefinitive response was received from the CWF requiring development (PIP reimbursement) K = A definitive response was not received from the CWF within seven days (delayed response) (non-PIP reimbursement) L = A definitive response was not received from the CWF within seven days (delayed response) (PIP reimbursement) M = The claim was manually set to ‘other.’ This will only occur in rare situations such as a claim required development external to the intermediary’s operation (non-PIP reimbursement) N = The claim was manually set to ‘other.’ This will only occur in rare situations such as a claim required development external to the intermediary’s operation (PIP reimbursement) O = The calm was a sequential claim in which the prior claim was pending and was determined ‘other’ (non-PIP reimbursement) P = The calm was a sequential claim in which the prior claim was pending and was determined ‘other’ (PIP reimbursement) |
| USER ACT | User action code– Used for medical review and reconsiderations only |
| TPTP A/B | Tape-to-tape flag Medicare Part A/B – indicates whether the claim was posted to the CWF Valid Values: Blank – claim posted to CWF X – claim did not post to CWF |
| NP CD A/B | Nonpayment code for Medicare Part A/B – identifies the reason for Medicare’s decision not to make payment (two-position alphanumeric field) |
| HD CPY A/B | Hard copy Medicare Part A/B – instructs the system to generate a specific hardcopy document during the claim process (one-position alphanumeric field) |
| NB ADR | Number of additional developmental requests – identifies the number of times an Additional Request form will be generated. If a second request is to be generated after the initial request is generated, a ‘2’ will appear in this field. If only a request is to be generated with no second request, a ‘1’ will appear in this field. |
| CAL DY | Calendar days – identifies the number of calendar days a claim is to suspend after the generation of an Additional Development Request. For example, if ‘30’ is entered in this field and ‘1’ is entered in the prior field (NB ADR), the claim suspends for 30 days after the generation of the first ADR form. At the end of 30 days if the requested information is not received, the system rejects the claim. If a second request is required to be generated 15 days after the original generation of the ADR form, a ‘2’ appears in the NB ADR field and ‘15’ in the CAL DY field. After generation of the initial request form, the claim suspends for 15 days and then generates the second request. The claim suspends another 15 days and if the requested information is not received within 15 days, the system rejects the claim (two-digit field) |
| C/L | Claim or line indicator – Identifies if the applicable action for a reason code is to be applied at claim level or line level (C—claim level, L—line level). |
| NARRATIVE | Displays the narrative for the reason code. Includes instructions for further actions required, as appropriate. |
The reason code narrative may extend several pages. To display additional narrative, press the <F6/PF6> key.
Additional information related to the reason codes assigned to a claim are available in the form of ANSI reason codes. These codes provide details describing the reimbursement status of a claim or claim line.
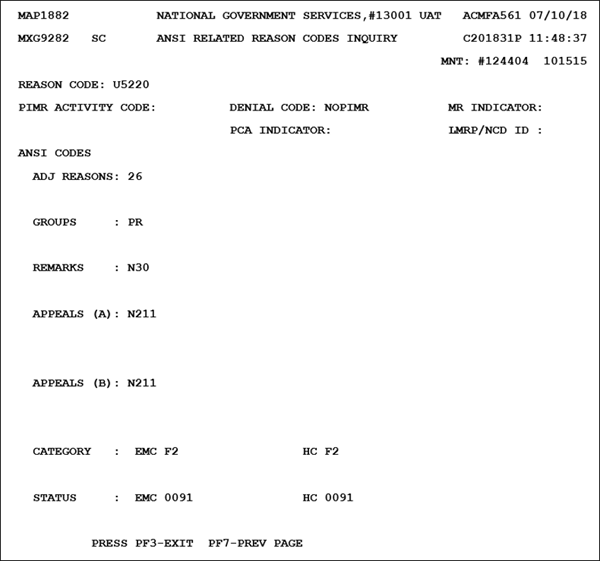
To review the ANSI information related to the reason code, press the <F8/PF8> key. The ANSI RELATED REASON CODES INQUIRY screen is available:
| Field | Description |
|---|---|
| REASON CODE | Reason code – identifies the FISS reason code for which the following ANSI codes relate. |
| PIMR ACTIVITY CODE | Identifies the PIMR activity code for which the reason code is being categorized (two-position alphanumeric field) Valid values: AI = Automated CCI edit AL = Automated locally developed edit AN = Automated national edit CP = Prepay complex probe review DB = TPL or demand bill claim review MR = Manual routine review PS = Prepay complex provider specific review RO = Reopening SS = Prepay complex service specific review |
| DENIAL CODE | Identifies the PIMR Denial Reason Code that is being categorized (six-position alphanumeric field) Valid values: 100001 = Documentation does not support service 100002 = Investigation/experimental 100003 = Item/services excluded from Medicare coverage 100004 = Requested information not received 100005 = Service not billed under the appropriate revenue or procedure code 100006 = Services not documented in record 100007 = Services not medically reasonable and necessary 100008 = SNF demand bills 100009 = Daily nursing visits are not intermittent/part time 100010 = Specific visits did not include personal care service 100011 = Home health demand bills 100012 = Ability to leave home unrestricted 100013 = Physician’s order not timely 100014 = Service not ordered/not included in treatment plan 100015 = Services not included in the plan of care 100016 = No physician certification 100017 = Incomplete physician order 100018 = No individual treatment plan 100019 = Other |
| MR Indicator | Identifies whether or not the service received Complex Manual MR (one-position alphanumeric field) Valid values: Y = Medical records received. This service received complex manual MR. N = Medical records were not received. This service received routine manual MR. Blank = The services did not receive manual MR. |
| PCA INDICATOR | Identifies the Progressive Correction Action indicator (one-position alphabetic field) Valid Values: Blank ‑ The Medical Policy Parameter is not PCA-related and is not included in the PCA transfer files. Y ‑ The Medical Policy Parameter is PCA-related and is included in the PCA transfer files. N ‑ The Medical Policy Parameter is not PCA-related and is not included in the PCA transfer files. |
| LMRPNCD ID | Identifies the LMRP and/or NCD identification numbers, which are assigned to the FMR reason code for reporting on the beneficiaries Medicare Summary Notice (11-position alphanumeric field, with five occurrences). The values for the LMRP are user defined and the NCD is CMS defined. |
ANSI Codes
| Field | Description |
|---|---|
| ADJ REASONS | This is the ANSI adjustment reason code that is related to the FISS reason code (three-position alphanumeric field, with ten occurrences). |
| GROUPS | Identifies the ANSI group codes (two-position alphanumeric field, with four occurrences). |
| REMARKS | Identifies the ANSI remark reason(s) for nonpayment (five-position alphanumeric field, with four occurrences). All reason codes with a status of ‘R’ or ‘D’ should contain at least one occurrence of the ANSI group, adjustment, remark (optional) and appeal codes based on the following:
|
| APPEALS (A) | ANSI appeal–A codes – These codes are used for inpatient only (five-position filed, with 20 occurrences) |
| APEPALS (B) | ANSI appeal–B codes – These codes are used for outpatient only (five-position field, with 20 occurrences) |
| CATEGORY EMC | EMC Claim Status Category Code – identifies the category status of the EMC claim that is returned on a 277 claim response |
| CATEGORY HC | Hard Copy Claim Status Category Code – identifies the category status of the hard copy claim that is returned on a 277 claim response |
| STATUS EMC | EMC Claim Status Code – identifies the status of the EMC-submitted claim that is returned on a 277 claim response. |
| STATUS HC | Claim status codes – identifies the status of the hard copy submitted claim that is returned on a 277 claim response. |
To further research ANSI reason codes, access FISS Inquiries Submenu ANSI REASON CODES (68).
Revised 8/16/2023