- Introduction
- Chapter I - Online System Terminology
- Chapter II - Online Menu Functions Overview
- Chapter III - Navigating the Online System
-
Chapter IV - Inquiries Submenu (01)
- Accessing the Inquiries Submenu
- Beneficiary/CWF (10)
- DRG (Pricer/Grouper) (11)
- Claim Summary (12)
- Revenue Codes (13)
- HCPCS Codes (14)
- DX/Proc Codes ICD-9 (15)
- Adjustment Reason Codes (16)
- Reason Codes (17)
- ZIP Code File (19)
- OSC Repository Inquiry (1A)
- Claim Count Summary (56)
- Home Health Payment Totals (67)
- ANSI Reason Codes (68)
- Invoice Number/DCN Translator (88)
- DX Proc Codes ICD-10 (1B)
- Community Mental Health Centers Services Payment Totals (1C)
- Check History (FI)
- Provider Practice Address Query (1D)
- New HCPCS Screen (1E)
- Opioid Use Disorder (OUD) Demo 99 (1F)
- Chapter V - Claims and Attachments Submenu (02)
- Chapter VI - Claims Correction Submenu (03)
- Chapter VII - Online Reports View Submenu (04)
-
Resources
- Part A Electronic Medicare Secondary and Tertiary Payer Specifications for ANSI Inbound Claim
- Electronic Medicare Secondary Payer Specifications for Inbound Claims
- FISS UB-04 Data Entry Payer Codes
- Common Claim Status/Locations
- FISS Reason Code Overview
- FISS Reason Code/Claim Driver Overview
- Program Function/Escape Key Crosswalk
- How to Adjust a Claim
- FISS Claim Change/Condition Reason Codes
- How to Cancel a Claim
- How to Correct a Return to Provider Claim
- Online System Menu Quick-Reference
Chapter VII: Online Reports View Submenu (04)
Credit Balance Report - CMS 838 (R3)
Purpose
Credit balance reporting is used to certify whether you have any outstanding monies owed to the Medicare Program. Part A providers submit credit balance reports to Medicare as they occur.
Providers may use the FISS Online Reports Credit Balance Report - CMS-838 option to disclose Medicare credit balances. This option allows users to submit the 838 detail page that identifies each credit balance.
Note: Only those credits for which the amount due to Medicare has not been recouped through the claim adjustment process should be reported on the 838 detail page.
To access the CREDIT BALANCE REPORT - CMS-838 option from the FISS system ONLINE REPORTS submenu, type ‘R3’ at the ENTER MENU SELECTION: prompt, then press <Enter>.
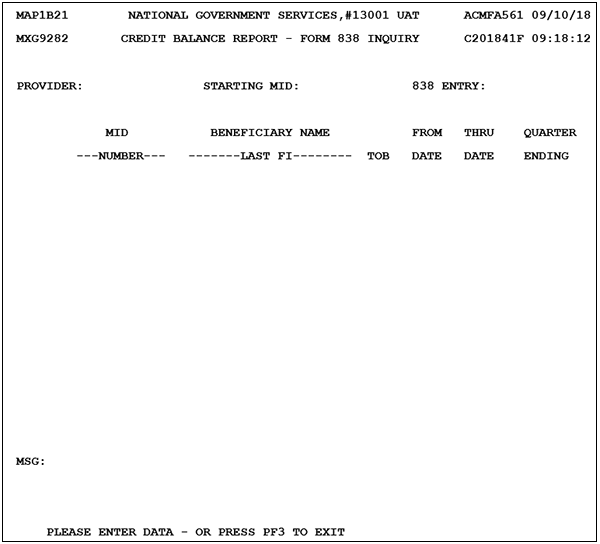
Upon selecting the CREDIT BALANCE REPORT - CMS-838 option, the CREDIT BALANCE REPORT – FORM 838 INQUIRY screen is available:
To begin a credit balance, type ‘Y’ in the 838 ENTRY: field, then press the <Enter> key. The CREDIT BALANCE REPORT – FORM 838 ENTRY screen is available:
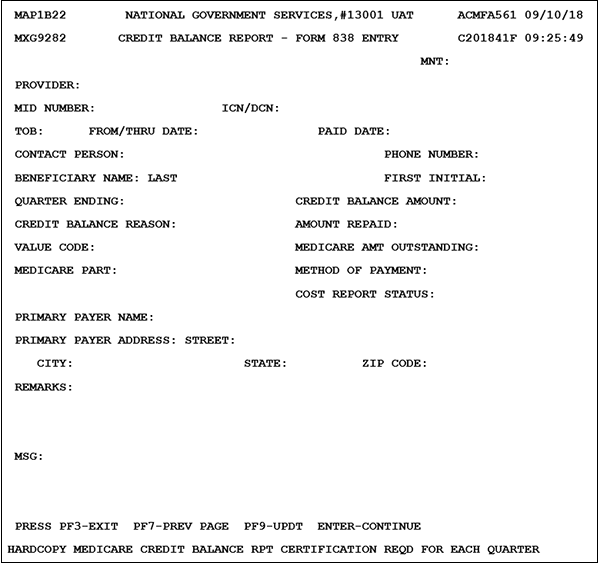
For each credit balance, enter the information requested by the fields included in the online CMS-838 form, then press the <F9/PF9> key:
| Field | Description |
|---|---|
| PROVIDER | Provider– the provider number of the institution who rendered services (auto-generated, 13-position alphanumeric field) |
| MID | Medicare ID number–the Medicare ID number assigned to the beneficiary by the CMS, to be used on all correspondence and to facilitate the payment of claims (12-position alphanumeric field) |
| ICN/DCN | ICN/DCN–internal claim number/document control number (23-position alphanumeric field) |
| TOB | Type of bill–type of facility, bill classification, and frequency of the claim (three-position numeric field) |
| FROM/THRU DATE | Statement from date–the beginning date of service for the period included on the claim (six-digit field in MMDDYY format) Statement through date–the ending date of service for the period included on the claim (six-digit field in MMDDYY format) |
| PAID DATE | Paid date–the scheduled payment date of the claim or the date the provider is actually reimbursed (six-digit field in MMDDYY format) |
| CONTACT PERSON | Contact person–the name of the contact person, at the provider's location (30-position alphabetic field) |
| PHONE NUMBER | Phone number–the contact person's phone number (10-position numeric field) |
| BENEFICIARY NAME: LAST | Beneficiary name: last–the beneficiary's last name (20-position alphabetic field) |
| FIRST INITIAL | First initial–the beneficiary's first initial (one-position alphabetic field) |
| QUARTER ENDING | Quarter ending–the quarter ending date (six-digit field in CCYYMM format) |
| CREDIT BALANCE AMOUNT | Credit balance amount–the credit balance amount (11-digit field in 999999999.99 format) |
| CREDIT BALANCE REASON | Credit balance reason–the credit balance reason (one-position numeric field) Valid values 1 = Duplicate payment 2 = Other insurance primary 3 = Other reason for credit balance |
| AMOUNT REPAID | Amount repaid–the repaid amount (11-digit field in 999999999.99 format) |
| VALUE CODE | Value code–the value code (two-position alphanumeric field) Valid values 12 = Working-aged with EGHP 13 = ESRD beneficiary in first-year coordination period 14 = Automobile, no-fault liability insurance 15 = Workers’ compensation 16 = VA, PHS, or other federal agency 41 = Black Lung 42 = VA 43 = Disabled beneficiary under 65 44 = Obligated to accept 47 = Any liability insurance Note: Values equate to a MSP value code. |
| MEDICARE AMT OUTSTANDING | Medicare amount outstanding–the outstanding Medicare amount (11-digit field in 999999999.99 format) |
| MEDICARE PART | Medicare Part– Identify whether the claim is Part A or Part B (one-position alphabetic field) Valid values A = Medicare Part A B = Medicare Part B |
| METHOD OF PAYMENT | Method of payment–the method of payment (one-position alphabetic field) Valid values A = Adjustment submitted hardcopy C = Check submitted X = Adjustment submitted hardcopy or electronically Z = Combination of check and adjustment submitted |
| COST REPORT STATUS | Cost report status–the cost report status (one-position alphabetic field) Valid values O = Open C = Closed |
| PRIMARY PAYER NAME | Primary payer name–the name of the primary payer (25-position alphanumeric field) |
| PRIMARY PAYER ADDRESS: STREET | Primary payer address street–the street address of the primary payer (30-position alphanumeric field) |
| CITY | Primary payer address city–the city of the primary payer (15-postiton alphabetic field) |
| STATE | Primary payer address state–the state of the primary payer (two-position alphabetic field) |
| ZIP CODE | Primary payer address ZIP Code–the ZIP Code of the primary payer (nine-position numeric field) |
| REMARKS | Remarks–remarks lines (67-position alphanumeric field) |
| MSG | Message–displays error messages (see list below, 73-position alphanumeric fields) |
Once the credit balance report CMS-838 form has been successfully entered, the screen will refresh to display “RECORD SUCCESSFULLY ADDED. PLEASE ENTER DATA – OR PRESS PF3 TO EXIT” in the MSG field.
An additional reminder also appears at the bottom of the screen, reminding you that the hardcopy Medicare Credit Balance Report Certification page should also be sent to complete submission of the Credit Balance Report.
Continue to enter information for each credit balance. Don’t forget to press the <PF9/F9> key to save and submit each CMS-838 form.
Credit Balance Error Messages
When an error has been encountered, the MSG field at the bottom of the screen will be updated. The following error messages will be displayed on the entry screen when an error is encountered:
- If a MID and DCN is not entered, return the following error message: “MID and DCN numbers required.”
- If a MID/DCN combination does not match a MID/DCN present in the FISS DDE, return the following error message: “No match for the MID and DCN numbers entered.”
- If a duplicate MID/DCN combination record is entered during the same report quarter, return the following error message: “Duplicate MID and DCN entered for same quarter.”
- If the TOB present is equal to ‘xx0’ (i.e., third digit = zero), return the following error message: “Type of bill for MID/DCN entered = xx0—no credit balance required.” FS5106—Add Credit Balance Process to System July 2008 Fiscal Intermediary Standard Systems 101”
- If the contact name and phone number information is not entered, return the following error message: “Contact name and phone number required.”
- If the phone number is entered with nonnumeric data, return the following error message: “Phone number must be numeric.”
- If the beneficiary name—last and first initial—is not entered, return the following error message: “Beneficiary last name and first initial required.”
- If the quarter ending date is entered with nonnumeric data, return the following error message: “Quarter end must be numeric.”
- If the quarter-ending date month do not equal to 03, 06, 09, or 12, return the following error message: “Quarter-end month must equal 03, 06, 09, or 12.”
- If the quarter-ending date year is greater than the current year, return the following error message: “Quarter-end year must be less than or equal to current year.”
- If the quarter-ending date entered is within the current quarter, return the following error message: “Credit balance report not allowed until quarter ends.”
- If the credit balance reason is equal to ‘1’ or ‘3,’ a Medicare amount outstanding cannot be present; or if the credit balance reason is equal to ‘2’ and the paid date is not greater than 60 days prior and a Medicare amount outstanding is present, return the following error message: “MED AMT outstanding invalid with bal reason 1, 3, or 2 & PDDT > 60 days prior.”
- If a credit balance amount is not entered, return the following error message: “Credit balance amount required.”
- If the credit balance amount is entered with nonnumeric data, return the following error message: “Credit balance amount must be numeric.”
- If the credit balance reason is equal to ‘1’ and the credit balance amount and amount repaid is not equal, return the following error message: “credit balance reason equals 1: credit balance amount and amount repaid must equal.”
- If the credit balance reason is equal to ‘1’ and an amount outstanding is present, return the following error message: “Credit balance reason equals 1: amount outstanding must equal zero.”
- If the credit balance reason is equal to ‘2’ and the value code, payer name, or address is blank, return the following error message: “Credit balance reason equals 2: value code, payer name and address required.”
- If the credit balance reason is equal to ‘3’ and the remarks are blank, return the following error message: “Credit balance reason equals 3: remarks required.”
- If the quarter-ending date entered is prior to the current quarter, return the following error message: “Quarter-ending date entered is prior to current quarter.”
- If the credit balance amount minus the amount paid is not equal to the amount outstanding, return the following error message: “Credit balance amount minus amount paid must equal amount outstanding.”
- If the amount repaid is nonnumeric, return the following error message: “Amount repaid must be numeric.”
- If the cost-report status field is not equal ‘O’ or ‘C,’ return the following error message: “Cost-report status invalid: valid values ‘O’ or ‘C’.”
- If the method of payment field is not equal to ‘A,’ ‘C,’’X’, or ‘Z,’ return the following error message: “Method of payment invalid: valid values ‘A,’ ‘C,’ ‘X,’ or ‘Z’.”
- If the method of payment is equal to ‘X’ and the credit balance amount and amount repaid values are not equal, return the following error message: “Method of payment = X: credit balance amount and amount repaid must equal.”
- If the Medicare amount outstanding field value is nonnumeric, return the following error message: “Medicare amount outstanding must be numeric.”
- If the credit balance reason is not equal to ‘1,’ ‘2’, or ‘3,’ return the following error message: “Reason for credit balance invalid: valid values ‘1,’ ‘2’, or ‘3’.”
- If the value code present is not equal to 12–16, 41, 42, 43, 44, or 47, return the following error message: “Value code, if present, must equal 12–16, 41, 42, 43, 44, or 47.”
- If the payer name and address is present and the credit balance reason is not equal to ‘2,’ return the following error message: “Payer name and address present: credit balance reason must equal ‘2’.”
- If the provider number entered is not valid, return the following error message: “Invalid provider number entered. Please reenter provider number.”
To review a list of Credit Balance CMS-838 forms that have been entered in the FISS system, press the <F3/PF3> key. From the FISS system ONLINE REPORTS submenu, type ‘R3’ at the ENTER MENU SELECTION: prompt, then press <Enter>.
The CREDIT BALANCE REPORT – FORM 838 INQUIRY screen will be populated with the MIDs that have been entered during the current quarter.
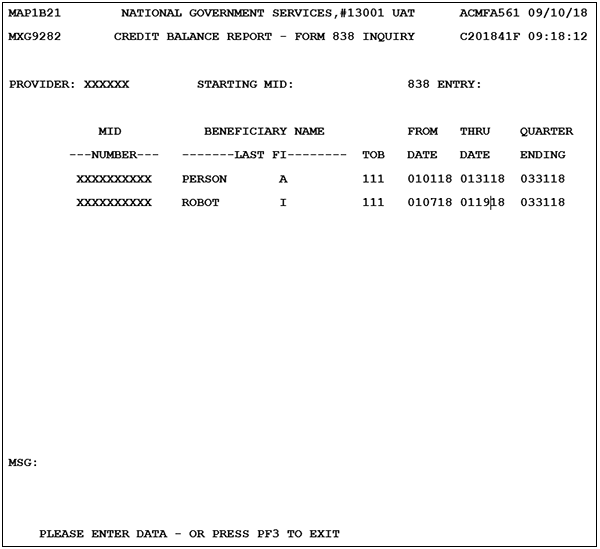
To review the details of a credit balance report, use the <Tab> key to advance to the Selection field.
Note: the Selection field is not labeled. The cursor will appear to the left of the MID number.
Enter ‘S’ in the Selection field, then press the <Enter> key to display the credit balance form
Enter ‘D’ in the Selection field, then press the <Enter> key to delete the credit balance form
Enter ‘U’ in the Selection field, then press the <Enter> key to update credit balance form. Remember to press the <PF9/F9> key to save and submit updates to the CMS-838 form.
Note: 30 days after the quarter-end date all available information will be removed.
Additional information on Credit Balance Reporting can be found on the Overpayments section of our website.
Revised 3/31/2025