- Introduction
- Chapter I - Online System Terminology
- Chapter II - Online Menu Functions Overview
- Chapter III - Navigating the Online System
-
Chapter IV - Inquiries Submenu (01)
- Accessing the Inquiries Submenu
- Beneficiary/CWF (10)
- DRG (Pricer/Grouper) (11)
- Claim Summary (12)
- Revenue Codes (13)
- HCPCS Codes (14)
- DX/Proc Codes ICD-9 (15)
- Adjustment Reason Codes (16)
- Reason Codes (17)
- ZIP Code File (19)
- OSC Repository Inquiry (1A)
- Claim Count Summary (56)
- Home Health Payment Totals (67)
- ANSI Reason Codes (68)
- Invoice Number/DCN Translator (88)
- DX Proc Codes ICD-10 (1B)
- Community Mental Health Centers Services Payment Totals (1C)
- Check History (FI)
- Provider Practice Address Query (1D)
- New HCPCS Screen (1E)
- Opioid Use Disorder (OUD) Demo 99 (1F)
- Chapter V - Claims and Attachments Submenu (02)
- Chapter VI - Claims Correction Submenu (03)
- Chapter VII - Online Reports View Submenu (04)
-
Resources
- Part A Electronic Medicare Secondary and Tertiary Payer Specifications for ANSI Inbound Claim
- Electronic Medicare Secondary Payer Specifications for Inbound Claims
- FISS UB-04 Data Entry Payer Codes
- Common Claim Status/Locations
- FISS Reason Code Overview
- FISS Reason Code/Claim Driver Overview
- Program Function/Escape Key Crosswalk
- How to Adjust a Claim
- FISS Claim Change/Condition Reason Codes
- How to Cancel a Claim
- How to Correct a Return to Provider Claim
- Online System Menu Quick-Reference
Chapter VII: Online Reports View Submenu (04)
About the 201 Pend Report
Purpose
The 201 Pend Report is designed to assist providers in accessing information regarding the status of their submitted claims. This report is available to view directly through the FISS DDE online system—this is a weekly report.
The 201 report has three main sections:
- Summary of Pended Claims;
- Summary of Processed Claims; and
- Summary of Returned Claims
Each summary section of the report provides a separate count for both original claims and adjustment claims. Each report section is labeled based on type of bill (TOB).
The last page of the 201 Pend Report contains a summary of the pended, processed, and returned sections. This page of the report is titled “Claims Summary Totals.”
The remainder of this section will address the information contained within each section of the 201 Pend Report, and will show you how the report will visually appear online.
Whenever you are viewing a report on the FISS DDE online system, you will need to toggle between a “left to right” viewing screen environment. To accomplish this, use the <PF11> key to move your viewing screen to the right, and the <PF10> key to return your viewing screen to the left.
Please note: Medicare Choice claims, end-stage renal disease (ESRD)-managed care demo claims, and plan submitted health maintenance organization (HMO) (Encounter) claims are excluded.
Summary of Pended Claims– First Report Section
Claims will remain on the SUMMARY OF PENDED CLAIMS section of the report until they are either paid, rejected, or return to provider (RTP).
The following two screen prints show how the SUMMARY OF PENDED CLAIMS section appears on the FISS DDE online system:
Summary of Pended Claims – Left View
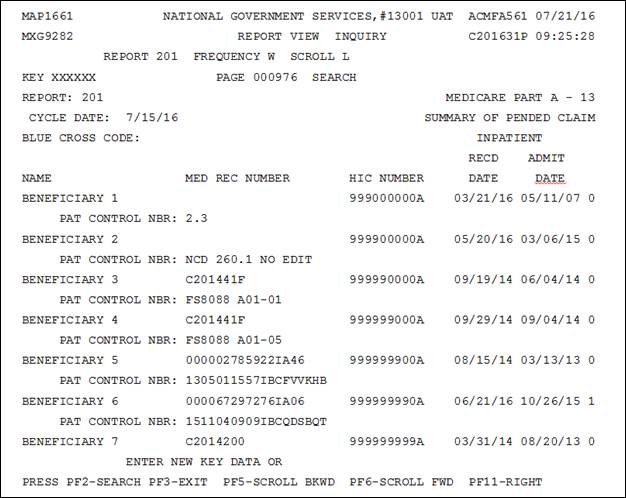
Summary of Pended Claims – Right View
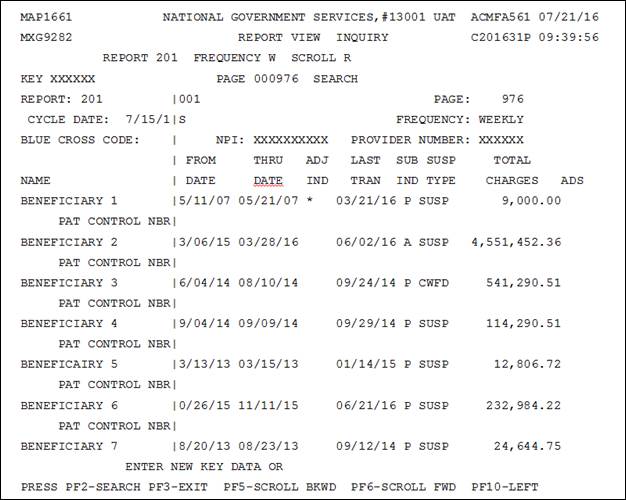
Summary of Pended Claims– Right View Field Descriptions
The following chart describes the various fields/report headings contained within the Summary of Pended Claims section of the 201 Pend Report.
| Field/Report Heading | Description |
|---|---|
| NAME | The patient’s name as you reported it |
| MEDICAL RECORD NUMBER | This is the medical record number given to National Government Services. If one is not given, the field should be blank. |
| HIC NUMBER | The patient’s Medicare number reported |
| RECD DATE | The day National Government Services received the claim |
| ADMIT DATE | Date from block 17 of the UB-04 |
| FROM DATE | Date from block 6 of the UB- 04 |
| THRU DATE | Date from block 6 of the UB- 04 |
| ADJ IND | An asterisk indicates that the claim is an adjustment, blank indicates an original claim |
| LAST TRAN | Last date that some activity occurred on the claim. |
| SUB IND | Valid values A = Claim submitted via electronic media claim (EMC) P = Claim submitted via paper |
| SUSP TYPE | Suspend type– Indicates why the claim is suspended. Valid Values MED = Medical Review MSP = Medicare Secondary Payer (MSP) CWFR = Common Working File (CWF) regular (these claims are in initial query to the CWF) CWFD = CWF delayed (the claim has been sent to CWF but has to be reprocessed so that it is no longer considered a “clean claim”) SUSP = General suspended claims Note: Some internal review of this document is necessary before it can be released for payment, rejection, or additional development. |
| TOTAL CHARGES | Charges as reported in column 47 of the UB- 04. |
| ADS | Additional development suspense– ‘Y’ indicates a request for additional information that has been generated to you by Medical Review, MSP, or the Claims Unit. On the next line of the report there should also be a reason code that will describe the information that National Government Services has requested via additional development request (ADR). |
The last page of each of the pended claims categories contains a summary of the total claim count and associated dollar amount for the corresponding SUSP TYPE. Totals are provided for both original claims and adjustment claims.
Summary of Processed Claims – Second Report Section
The processed claims identified in this section of the 201 Pend Report are those that we have adjudicated through the FISS DDE to a point of completion.
The following two screen prints show you how the SUMMARY OF PROCESSED CLAIMS section appears on the FISS DDE online system.
Summary of Processed Claims – Left View
Summary of Processed Claims – Right View
Summary of Processed Claims – Right View
The fields/report headings contained within the SUMMARY OF PROCESSED CLAIMS section of the 201 Pend Report are the same as for the PENDED CLAIMS section, with the exception of the last three. These fields are:
| FIELD/REPORT HEADING | DESCRIPTION |
|---|---|
| PAID DATE | The date the claim was finalized or the date of remittance advice on which the paid claim will appear. All of the paid claims will appear in this report only once. The rejected or denied claim will also appear only once on this report. |
| CLEAN IND | This code will be an alpha A–P, a code D may indicate interest payment due. Valid values A = Periodic interim payment (PIP) other B = PIP clean C = Non-PIP other D = Non-PIP clean E = Additional information requested-non-PIP F = Additional information requested-PIP G = Date of death response received from host-non-PIP H = Date of death response received from host-PIP I = Nondefinitive reply-non-PIP J = Nondefinitive reply-PIP K = Delayed response-non-PIP L = Delayed response-PIP M = Manually set to nonclean-non-PIP N = Manually set to nonclean-PIP O = Sequential claim in which prior pending claim-non-PIP P = Sequential claim in which prior pending claim-PIP |
| REJECT CODE | If the claim is rejected, a code will appear. For some rejections, there will also be a letter to you and to the beneficiary. |
The last page of each of the processed claim categories identifies the total number of claims and adjustments.
Summary of Returned Claims– Third Report Section
This section is of particular importance to providers because it identifies all claims that are being returned to the provider or RTP. If a claim appears on this section of the 201 Pend Report, it is no longer considered in the FISS DDE claim inventory (i.e., it is no longer in our system.) Claims identified in this section will never be adjudicated for payment, rejection, or denial unless the provider either:
- corrects the claim through the online system; or
- resubmits the claim through normal billing channels.
Claims will appear only once on the SUMMARY OF RETURNED CLAIMS section.
The following two screen prints show how the SUMMARY OF RETURNED CLAIMS section appears on the FISS DDE online system:
Summary of Returned Claims – Left View
Summary of Returned Claims – Right View
The fields/report headings contained within the Summary of Returned Claims section of the 201 Pend Report are the same as for the Pended Claims section, with the exception of the last two. These fields are the following:
| Field/Report Heading | Description |
|---|---|
| RTP DATE | The date the claim was returned to the provider for correction. |
| RTP REASON CODE | States why the claim has been returned. Locate the code and follow the instructions to correct and resubmit the claim. |
The last page of each of the returned claims categories identifies the total number of claims and adjustments that have been RTP.
CLAIMS SUMMARY TOTALS– Last Page of the 201 Pend Report
This last page of the 201 Pend Report provides a summary of the total claim counts associated with the pended, processed, and returned claims sections.
The following two screen prints show you how the CLAIMS SUMMARY TOTALS page appears on the FISS DDE online system:
Claims Summary Totals - Left View
Claims Summary Totals – Right View
Revised 7/29/2016