- Avoiding Reason Code 38200
- Correcting Reason Code 37253
- Incarcerated or Unlawfully Present in the U.S. Claim Rejections (U538H, U538Q)
- Expanded Home Health Value-Based Purchasing Model
- Billing the Home Health Period of Care Claim - PDGM
- Disposable Negative Pressure Wound Therapy Services Under Home Health
- Home Health Prospective Payment System Booklet
- Home Health Third Party Liability Demand Billing
- Home Health Demand Billing
- Notice of Admission Questions and Answers
- Billing the Home Health Notice of Admission Electronically
- Billing the Home Health Notice of Admission via DDE
- Home Health Transfers
- Home Health Agency Transfer and Dispute Protocol
- Late Notice of Admission - The Exception Process
- Reporting Home Health Periods with No Skilled Visits
- Telehealth Home Health Services
- Reporting Site of Service Codes for Home Health Care
- PDGM Resources
- Billing G-Codes for Therapy and Skilled Nursing Services
- Correcting and Avoiding Reason Code 38157: Duplicate Request for Anticipated Payment
- Correcting and Avoiding Reason Code C7080: Inpatient Overlap
- Completing the Advance Beneficiary Notice for Home Health Agency Demand Claims
- The Medicare Home Infusion Therapy Benefit and Home Health Agencies
- Home Health Therapy Billing
- Home Health Billing When a New MBI is Assigned
- 30-Day Home Health Therapy Reassessment Schedule
Billing the Home Health Notice of Admission via DDE
Table of Contents
- Billing the Home Health Notice of Admission via DDE
- NOA Claim Page 1
- NOA Claim Page 4
- Related Content
Billing the Home Health Notice of Admission via DDE
Any codes within this job aid indicate common codes for required fields on Home Health NOAs. The NUBC maintains the coding information for Medicare billing, including the UB-04 data elements. For an all-inclusive listing of codes appropriate for all claim fields used for Medicare billing, visit the NUBC website to subscribe to the Official UB-04 Data Specifications Manual.
The bolded fields on the claim screen shots provided are the fields required when billing the Home Health NOA via Direct Data Entry (DDE). The tables below the screen shots include field title descriptions and the associated valid values.
NOA Claim Page 1
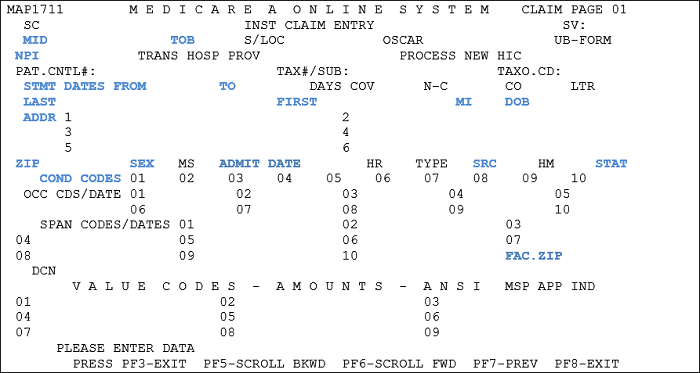
| Field | Description/Notes |
|---|---|
| MID Medicare ID Number |
Enter the Medicare Beneficiary Identifier |
| TOB Type of Bill |
32A – Notice of Admission 32D – Cancellation of Admission – You must choose the NOE/NOA option (49) in Claims Entry and change the bill type to ‘32D’ when cancelling |
| NPI National Provider Identifier Number |
Enter your home health agency’s NPI number. |
| STMT DATES FROM and TO (Statement Covers Period "From and "Through") | Report the date of the first visit provided in the admission as the From date. The "To" or "Through" date on the NOA must always match the "From" date. |
| LAST, FIRST, MI, ADDR, DOB, SEX | Patient’s last name, first name, and middle initial (if applicable), full address, date of birth (MMDDYYYY) and sex code (M/F) |
| ADMIT DATE | Enter the effective date of admission, which is the first Medicare billable visit and the Medicare start of care date (MMDDYY). The Admission date on the NOA must always match the From date. |
| SRC Source of Admission |
Submit a default value of "1." |
| STAT Patient Status |
Submit default value of "30." |
| COND CODES Condition Codes |
Enter condition code 47 for a patient transferred from another HHA. HHAs can also use cc 47 when the patient has been discharged from another HHA, but the discharge claim has not been submitted or processed at the time of the new admission. |
| FAC. ZIP | Facility ZIP Code of the provider or subpart (9 digit code). |
NOA Claim Page 4
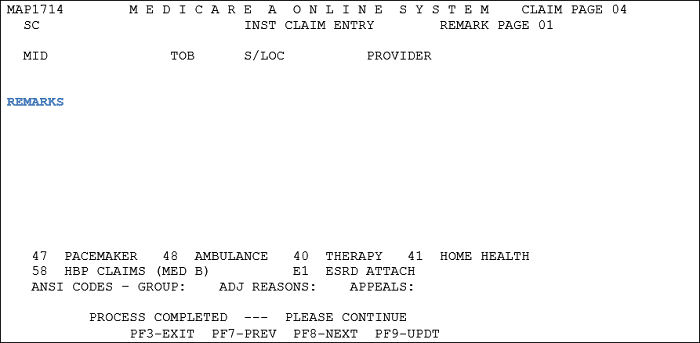
| Field | Description/Notes |
|---|---|
| REMARKS | Remarks are not required on the NOA; however, remarks are recommended when canceling the NOA to indicate the reason for cancellation. |
Notes:
- Required for any period of care that starts on or after 1/1/2022
- HHAs are to submit the NOA when they have received the appropriate physician’s written or verbal order that contains the services required for an initial visit, and the HHA has conducted the initial visit at the start of care
- NOA must be submitted within five calendar days from the start of care. A payment reduction applies if an HHA does not submit the NOA within this timeframe.
- Reduction in payment amount would be equal to a 1/30th reduction to the wage-adjusted 30-day period payment amount for each day from the home health start of care date until the date the HHA submitted the NOA
- The reduction would include any outlier payment
- The reduction amount will be displayed with value code QF on the claim
- Reduction in payment amount would be equal to a 1/30th reduction to the wage-adjusted 30-day period payment amount for each day from the home health start of care date until the date the HHA submitted the NOA
- When cancelling the NOA, all entered fields must exactly match the processed NOA
Related Content
Disclaimer: This job aid is not a legal document and is a collaboration between NGS, CGS and Palmetto GBA.
Reviewed 6/23/2025