- Avoiding Reason Code 38200
- Correcting Reason Code 37253
- Incarcerated or Unlawfully Present in the U.S. Claim Rejections (U538H, U538Q)
- Expanded Home Health Value-Based Purchasing Model
- Billing the Home Health Period of Care Claim - PDGM
- Disposable Negative Pressure Wound Therapy Services Under Home Health
- Home Health Prospective Payment System Booklet
- Home Health Third Party Liability Demand Billing
- Home Health Demand Billing
- Notice of Admission Questions and Answers
- Billing the Home Health Notice of Admission Electronically
- Billing the Home Health Notice of Admission via DDE
- Home Health Transfers
- Home Health Agency Transfer and Dispute Protocol
- Late Notice of Admission - The Exception Process
- Reporting Home Health Periods with No Skilled Visits
- Telehealth Home Health Services
- Reporting Site of Service Codes for Home Health Care
- PDGM Resources
- Billing G-Codes for Therapy and Skilled Nursing Services
- Correcting and Avoiding Reason Code 38157: Duplicate Request for Anticipated Payment
- Correcting and Avoiding Reason Code C7080: Inpatient Overlap
- Completing the Advance Beneficiary Notice for Home Health Agency Demand Claims
- The Medicare Home Infusion Therapy Benefit and Home Health Agencies
- Home Health Therapy Billing
- Home Health Billing When a New MBI is Assigned
- 30-Day Home Health Therapy Reassessment Schedule
Billing the Home Health Period of Care Claim – PDGM
Table of Contents
- Billing the Home Health Period of Care Claim – PDGM
- Claim Page 1:
- Claim Page 2:
- Claim Page 3
- Claim Page 4
- Claim Page 5
- Related Resources
Billing the Home Health Period of Care Claim – PDGM
Any codes within this job aid indicate common codes for required fields on Home Health claims. The NUBC maintains the coding information for all medical billing including the UB-04 data elements. For an all-inclusive listing of codes appropriate for all claim fields used for Medicare billing, visit the NUBC website for subscription to the UB-04.
The bolded fields on the claim screen shots provided are the fields required in billing the Home Health period of care claim. The tables below the screen shots include field title descriptions and the associated valid values.
HHA must submit an NOA at the beginning of an admission period and submit a claim for each 30-day period of care. Claims submitted before an NOA has been received for the beneficiary will be returned to the provider.
Claim Page 1:
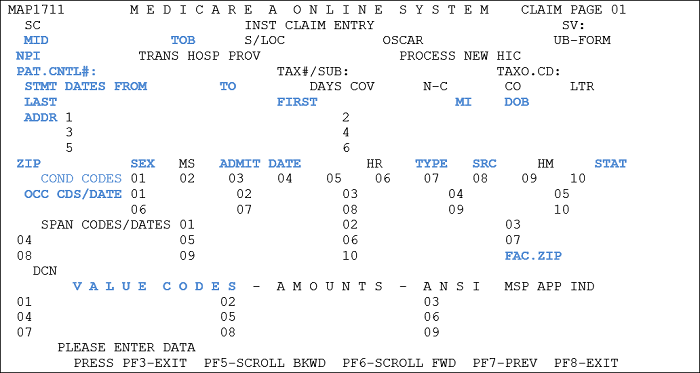
| Field | Description/Notes |
|---|---|
| MID | Medicare ID Number – Enter the Medicare Beneficiary Identifier |
| TOB | Type of Bill 329: Final Claim for an HH PPS Period – This code indicates an HH original bill to be processed following the submission of an HH PPS Notice of Admission (TOB 032A) 327: Replacement of Prior Claim – HHAs use to correct a previously submitted bill. Apply this code for the corrected or “new” bill. These adjustment claims must be accepted at any point within the timely filing period after the payment of the original claim. 328: Void/Cancel of a Prior Claim – HHAs use this code to indicate this bill is an exact duplicate of an incorrect bill previously submitted. A replacement claim must be submitted for the period of care to be paid. |
| NPI | National Provider Identifier Number |
| PAT. CNTL# | Patient Control Number – enter the number assigned to the patient’s medical/health record. |
| STMT DATES FROM and TO (Statement Covers Period "From and "Through") |
Enter the beginning and ending date of the period covered by the claim. The “From” date must be the first day of the period. MM/DD/YY format. The “From” date on an initial period must match the NOA date. The “To” date is either the date of discharge, transfer, or (for continuous care periods) 29 days after the “From” date. MMDDYY format. |
| LAST, FIRST, MI, ADDR, DOB, SEX | Patient’s last name, first name, and middle initial (if applicable), full address, date of birth (MMDDYYYY) and sex code (M/F) |
| ADMIT DATE |
The HHA enters the same date of admission that was submitted on the NOA for all periods until the patient is discharged (MMDDYY). |
| TYPE | Enter the appropriate NUBC code for the admission type. |
| SRC | Source of Admission – Enter the appropriate NUBC code for the source of admission. |
| STAT | Patient Status – Enter the code that most accurately describes the patient’s status as of the “To” date of the billing period. Any applicable NUBC approved code may be used. |
| COND CODES (Optional field) |
Some period claims may be billed with condition code 54 if there are no skilled services being billed, but there is a policy exception that allows billing covered services (e.g., home health aide services, medical social worker visits). |
| OCC CDS/DATE | Occurrence Codes and corresponding date (MMDDYY format): Enter Occurrence Code 50 with OASIS completion date (OASIS item M00900) Enter Occurrence Code 61 if there is a hospital discharge date within 14 days of HHA admission Enter Occurrence Code 62 if there is an other institutional discharge date (SNF, IRF, LTCH, or IPF) within 14 days of HHA admission |
| FAC. ZIP | Facility Zip Code of the provider or subpart (9 digit code). |
| VALUE CODES | Enter Value Code 61 with the appropriate Core Based Statistical Area (CBSA) Code. The five-digit CBSA code must be entered with two trailing zeroes. Enter Value Code 85 with the appropriate Federal Information Processing Standards (FIPS) code. The five-digit FIPS code must also be entered with two trailing zeroes. Note: CBSA codes can be found in the wage index file attached to the final rule. Each year, the Home Health Final Rule is linked to the Home Health Agency Center page on the CMS website. |
Claim Page 2:
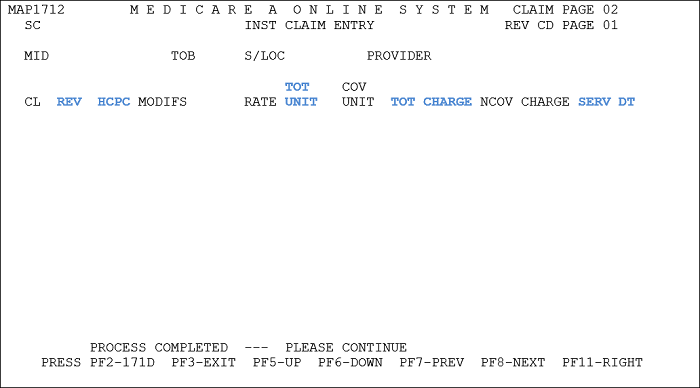
| Field | Description/Notes |
|---|---|
| REV | Revenue Codes – Claims must report a Revenue Code line 0023 to indicate billing under HH PPS. HHAs must also report revenue lines for all services provided to the patient within the period. |
| HCPC | The HIPPS code reported on the 0023 revenue line can be the HIPPS code the HHA expects will be used for payment if choosing to run grouping software for internal accounting purposes. If not, the HHA may submit any valid HIPPS code in order to meet this requirement. For all other revenue lines, report HCPCS codes as appropriate for each revenue code. |
| MODIFS | Modifiers – If the NOA that corresponds to a claim was filed late and the HHA is requesting an exception to the late-filing penalty, append modifier KX to the HIPPS code reported on the 0023 revenue code line. |
| SERV DT | Service Date – For initial periods of care, report the date of the first covered visit provided during the period on the 0023 revenue line. For subsequent periods, report the date of the first service provided under the HIPPS code reported on the 0023 revenue line, regardless of whether the visit was covered or noncovered. Report all other service dates for additional revenue codes as appropriate. MMDDYY format. |
| TOT UNITS | Total service units – No units of service are required on the 0023 revenue line. Units of service for other revenue codes are reported as appropriate. |
| TOT CHARGE | Total Charges – The total charge for the 0023 revenue line must be zero. Total charges for other Revenue Codes are reported as appropriate. |
| NCOV CHARGE (Optional Field) |
Noncovered Charges – Report total noncovered charges related to the revenue line. Examples of noncovered charges on HH PPS claims may include:
|
Claim Page 3
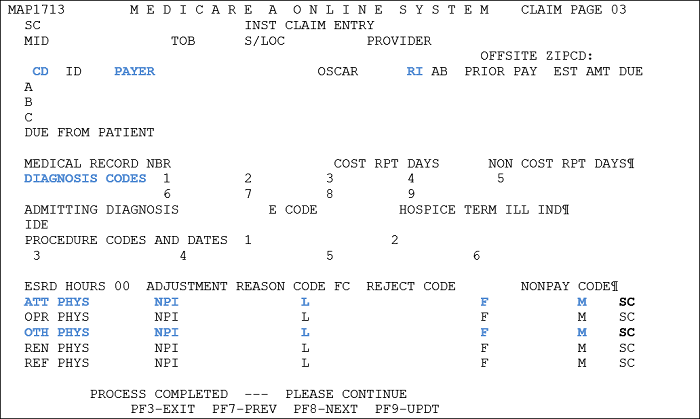
| Field | Description/Notes |
|---|---|
| PAYER | Payer Identification – If Medicare is the primary payer, enter “Medicare” on line A with payer code ‘Z’. Enter appropriate payer information for MSP situations. |
| RI | Release of Information – Entering “Y”, “R” or ‘’N” “Y” – Indicates the HHA has a signed statement on file permitting it to release data to other organizations in order to adjudicate claims “R” – Indicates the release is limited or restricted “N” – Indicates no release is on file |
| DIAGNOSIS CODES | Enter the appropriate ICD code for the principal diagnosis code and any other diagnosis codes (up to 24 additional codes) to accurately record what is driving patient care. The diagnosis codes on the period claim may not always match the OASIS. |
| ATT PHYS | Attending Physician – Enter the NPI and name (last name, first name, middle initial) of the attending physician who signed the plan of care – this must be the individual physician’s NPI, not a group NPI. The physician NPI in this field must be in PECOS as an eligible specialty to order and refer services under the home health benefit. |
| OTH PHYS | Name and NPI of the physician who certifies/recertifies the patient’s eligibility for home health care (this field only needs to be completed if the physician who certifies/recertifies is different than the physician who signs the plan of care). The individual physician NPI in this field must be in PECOS as an eligible specialty to order and refer services under the home health benefit. |
Claim Page 4
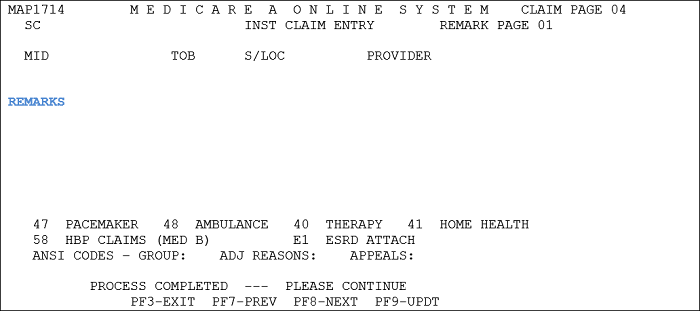
| Field | Description/Notes |
|---|---|
| REMARKS |
Remarks are not required on the claim; however, remarks are recommended when canceling/adjusting a claim to indicate the reason for cancellation/adjustment. |
Claim Page 5
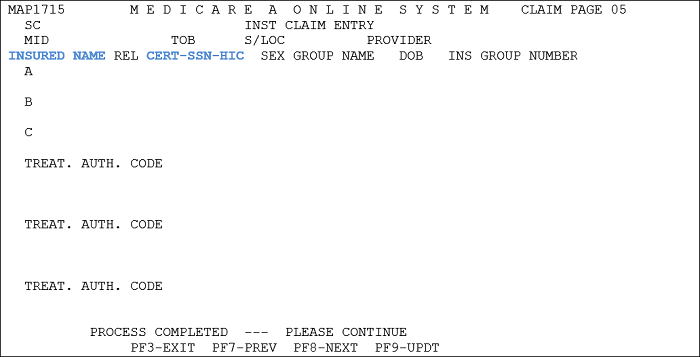
| Field | Description/Notes |
|---|---|
| INSURED NAME | Enter the patient’s name as shown on the Medicare card (or the information for the primary insurer in MSP situations). |
| CERT/SSN/HIC | Enter the Beneficiary’s Medicare number (or insured information for MSP claims) as it appears on the Medicare card if it does not automatically populate. |
Related Resources
There are chapters that include billing instructions for specific disciplines. These can be found within certain Publications in the CMS IOM:
- Information on billing as it specifically relates to Home Health can be found in CMS IOM Pub. 100-04, Medicare Claims Processing Manual, Chapter 10
- Information on billing Medicare Secondary Payer can be found in the CMS IOM Pub. 100-05, Medicare Secondary Payer Manual
- MSP information can also be found here on our website.
Reviewed 6/23/2025