- Medical Review Portal in NGSConnex
- Best Practices for a Successful Targeted Probe and Educate Review
- Medical Documentation Signature Requirements
- Address Corrections for Providers
- Additional Developmental Request Letters Overview
- How to Find and Respond to TPE ADR
- Methods for Responding to an ADR
- Sample TPE Notification Letter
- Sample TPE Notification Letter
- Results Letters
- Appeals
Sample TPE Notification Letter
Mail Date
Provider Name
Provider Address
City, State, Zip
Casefolder ID: Casefolder ID
Provider Number PTAN: PTAN (Provider Transaction Access Number)
Provider Number NPI: NPI (National Provider Identifier)
RE: Notice of Review - Targeted Probe and Education
Dear Medicare Provider, Supplier or Compliance Officer,
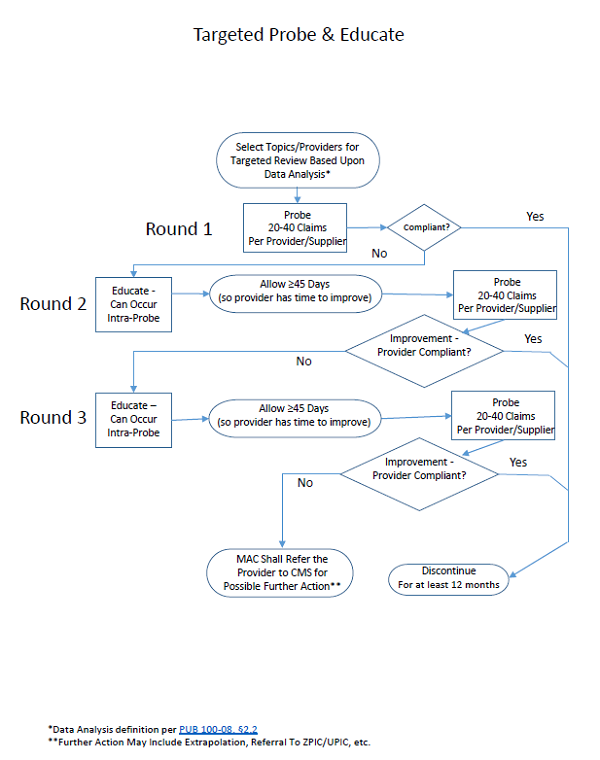
As part of our contractual obligation with the Centers for Medicare & Medicaid Services (CMS), National Government Services, Inc., your Jurisdiction 6 or K Medicare Administrative Contractor (MAC) performs Targeted Probe and Educate (TPE) to analyze provider compliance with CMS regulatory requirements. The TPE review process includes up to three rounds of a claim review with opportunities for education throughout the process. Discontinuation of this TPE review may occur at any time if provider compliance is demonstrated. If there are continued high denials after three rounds, National Government Services, Inc. will refer you to CMS for additional action, which may include 100% prepay review, extrapolation and/or referral to a Recovery Auditor.
This letter serves as notification that you have been selected to participate in a TPE review. This review aims to ensure your documentation supports the reasonable and necessary criteria of the services billed and follows Medicare rules and regulations.
Reason for Review
Provider Name was selected for review based on MR review reason. A prepayment review has been initiated to probe a sample of your claims (approximately 20-40 claims) billed with the following services rendered code(s):
- Service description and any related procedure code/HCPCS (Healthcare Common Procedure Coding System) code
Additional Documentation Requests
Please do not send any documentation at this time. You will be notified with an Additional Documentation Request (ADR) letter on each claim selected for review. This ADR letter will include the National Provider Identifier (NPI) of the provider rendering the service. It will also include a list of specific elements needed to support the service on review, such as:
- Physician/nonphysician practitioner’s progress notes
- History and physical examination notes with relevant medical history
- Physician’s orders
- Medication Administration Records
- Procedure/operative reports
- Relevant diagnostic findings or reports or documentation of time that would assist in supporting the services submitted
- Any additional documentation verifying medical necessity of the services submitted
- Legible signature/sample signature log/signature key/signature page, etc. to affirm the provider signature.
Please note, the ADR is two sided and may include more than one date of service.
Please ensure the process for routing these documents to the person(s) responsible for submission is timely and effective. Inform your staff responsible for receiving the ADR letters and submitting the required documentation for this review. Authorization for the collection of this information is included in Federal Law at SSA 1833 (e) and in Federal Regulation at 42 CFR 424.5(a)(6).
If you choose to fax your documentation, for optimal turn-around time, it is recommended that you separate fax transmissions for each individual beneficiary including the ADR letter followed by any related/requested documentation, i.e., one fax per ADR and bene. Please do not submit in bulk faxes, return each request individually; if you do not have the original ADR please attach a cover sheet with the beneficiary name.
If the requested documentation is not returned within 45 days, the claim will be denied due to a lack of documentation, which will contribute to your error rate. It is your responsibility as a provider to provide the requested documentation within he allotted time frame. Additionally, if you do not respond to the ADR request, MACs have the option to refer you to the Recovery Audit Contractor (RAC) or Zone Program Integrity Contractor (ZPIC)/Unified Program Integrity Contractor (UPIC) as a result. After all claims selected for the probe are reviewed, you will receive a letter that includes specific findings of our review.
Probe Completion
Upon completion of the medical review of all submitted claims, you’ll receive a results letter summarizing the findings, explaining any future actions and providing contact information to schedule a 1:1 educational session regarding the claim review results. This letter will include the number of claims reviewed; the number of claims allowed in full, the number of claims denied in full or in part and claim level education on the results. You may receive a claim remittance advice (RA) prior to the results letter. The date on the RA is considered the date of the initial claim decision. To exercise your right to an appeal, you must file a request in writing within 120 days from the date of the initial decision on the claim. Refer to the NGS website (www.ngsmedicare.com) for information about the Appeals Process and the Medicare Redetermination Request Form CMS-20027.
We remind you that CMS regulation at 42 CFR § 424.535 authorizes us to revoke Medicare billing privileges under certain conditions. In particular, we note that per 42 CFR § 424.535(a)(8)(ii), CMS has the authority to revoke a currently enrolled provider or supplier’s Medicare billing privileges if CMS determines the provider or supplier has a pattern or practice of submitting claims that fail to meet Medicare requirements.
In Closing
Thank you for your participation in this review. Upon receipt of this letter, please email Email Address with the name, phone number and email address for the contact person in your facility or office for this review. In the subject line, please include “Contact information for – Case Number – Casefolder ID number and your provider PTAN - PTAN.”
Sincerely,
Medical Review Manager Name
Jurisdiction K or 6 – Part B Medical Review Manager
National Government Services, Inc.
Revised 2/27/2024