- Tip Sheet for Medicare Providers on First Level of Appeals (Redeterminations)
- Tip Sheet for Medicare Providers on First Level of Appeals (Redeterminations)
- Tip Sheet for Medicare Providers on First Level of Appeals (Redeterminations)
- About Appeals
- About Appeals
- About Appeals
- Reopening versus Redetermination
- Who May File an Appeal
- Who May File an Appeal
- Who May File an Appeal?
- Who May File an Appeal?
- Levels of Appeals and Time Limits for Filing
- What Documents are Needed
- What Documents are Needed
- MSP Overpayments
- Submit an Adjustment to Correct Claims Partially Denied by Automated LCD-NCD Denials
- What Documents are Needed
- Submit an Appeal Electronically with NGSConnex
- Submit an Appeal Electronically via esMD
- Initiate Part B Reopenings or Non-MSP Overpayment Adjustments in NGSConnex
- Submit an Appeal Electronically via esMD
- What Documents are Needed
- Submit an Appeal Electronically via esMD
- Get Help Submitting an Appeal Hard Copy
- Get Help Submitting an Appeal Hard Copy
- Get Help Submitting an Appeal Hard Copy
- Submit an Appeal Electronically with NGSConnex
- Submit an Appeal Electronically via esMD
- Get Help Submitting a Appeal Hard Copy
- How to Prevent Duplicate Appeal and Clerical Error Reopening Requests in NGSConnex
- How to Avoid Costly Appeals
How to Prevent Duplicate Appeal and Clerical Error Reopening Requests in NGSConnex
Do you currently submit your appeal requests and reopening requests through NGSConnex? If so, did you know you are required to verify whether a request was previously submitted via NGSConnex, before submitting another request? Filing duplicate requests will result in processing delays and is abusive and costly to the Medicare program. We ask that you please refrain from sending duplicate appeal or clerical error reopening request.
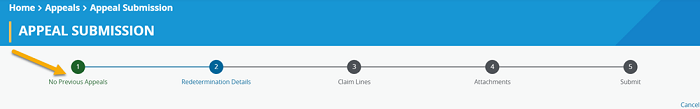
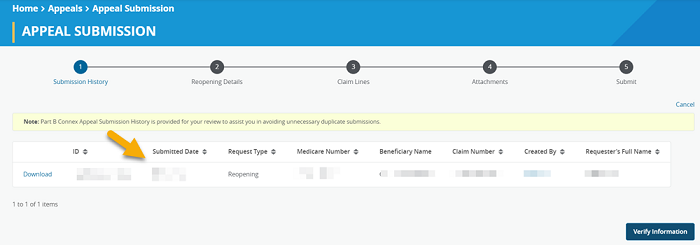
In NGSConnex when you initiate a clerical error reopening or redetermination the first step in the process is to verify Submission History. The Submission History panel will display any appeal request or clerical error reopening submitted via NGSConnex on or after 2/25/2022 by the provider selected. If you are unsure whether an appeal or clerical error reopening has been submitted for the claim selected and the Submission History is blank, and if Step 1 in the progress bar indicates ‘No Previous Appeals’, you should cancel and check appeal status before initiating a new request.
If the Submission History panel displays a previous submission and more than 60 days have passed since the appeal was submitted you should cancel the request and check appeal status. If less than 60 days have passed since the appeal was submitted you should cancel the request and wait until 60 days have passed and check appeal status.
If you do not agree with the outcome of a clerical error reopening or an appeal decision it is not appropriate to submit a duplicate request. You must follow the Medicare appeals process which is outlined in CMS IOM Publication 100-04, Medicare Claims Processing Manual, Chapter 29, Section 310.
Reviewed 11/25/2024
Helpful Resources
Log Into NGSConnex
Appeals Timeline Calculator
YouTube Video: Holistic Approach to Avoiding Administrative Burden
Form(s) you'll need: